Complete Guide to Effectively Managing Ulcerative Colitis: Symptoms, Treatments, and Lifestyle Strategies
This comprehensive guide explores ulcerative colitis management, covering symptoms, medications, lifestyle strategies, and surgical options. It highlights the importance of personalized treatment plans, hospital care for severe cases, and ongoing monitoring to maintain remission and prevent complications. Learn how to effectively manage this chronic condition through informed healthcare practices and lifestyle choices.
Understanding and Managing Ulcerative Colitis: A Comprehensive Approach
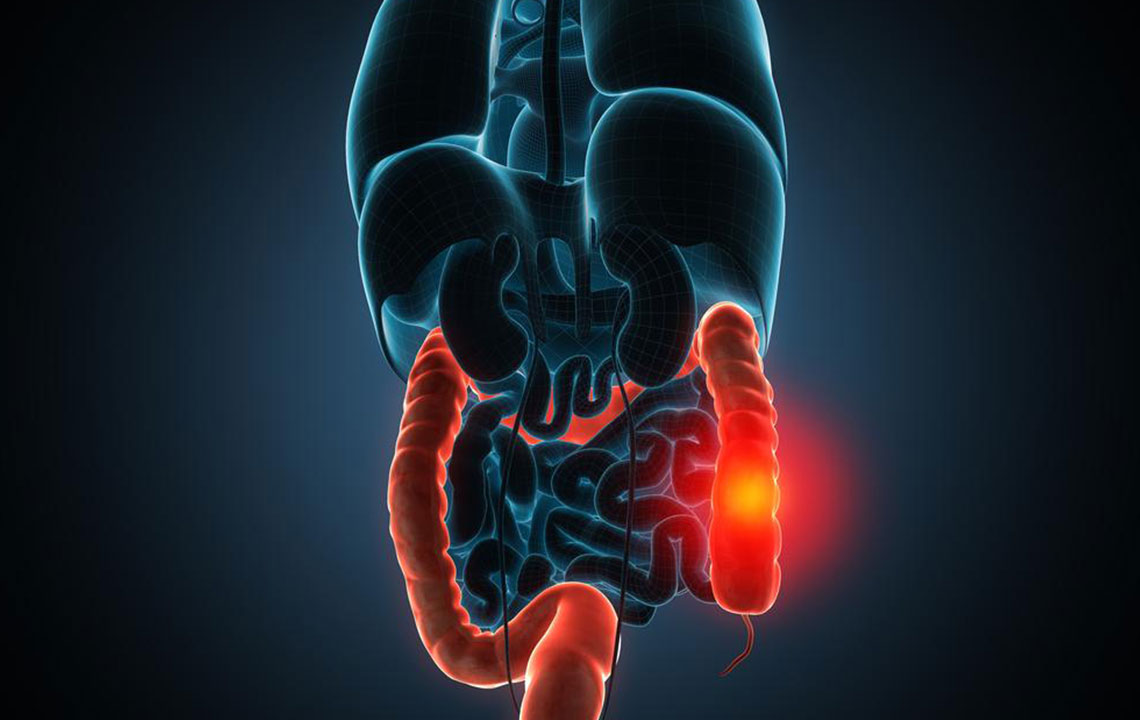
Ulcerative colitis is a chronic inflammatory disease that affects the innermost lining of the large intestine (colon) and rectum. This condition is characterized by the development of ulcers and sores on the colon’s surface, leading to symptoms such as abdominal pain, frequent diarrhea, blood in stool, and weight loss. Managing ulcerative colitis effectively involves a combination of medical treatment, lifestyle modifications, dietary management, and sometimes surgical intervention. The goal of treatment is to reduce inflammation, manage symptoms, prevent complications, and achieve long-term remission.
Medical Treatments for Symptom Control and Remission
Healthcare professionals typically recommend a personalized treatment plan based on disease severity, extent of colon involvement, and patient overall health. Common medications include:
Antidiarrheal agents: Medications like loperamide help control diarrhea and reduce urgency.
Medicated Enemas and Suppositories: These deliver anti-inflammatory drugs directly to the affected area, providing relief from localized inflammation.
Aminosalicylates: Drugs such as mesalamine or sulfasalazine are frontline treatments that reduce inflammation in the colon lining, helping to induce and maintain remission.
Steroids: Corticosteroids like prednisone are used during active flare-ups to quickly reduce inflammation, but are typically used for short-term control due to potential side effects.
Once inflammation subsides, doctors often continue aminosalicylates to sustain remission and prevent relapses. In addition to these standard treatments, several other therapeutic options are available:
Immunomodulators: Medications such as cyclosporine and azathioprine modulate the immune response to reduce ongoing inflammation. They are often prescribed for moderate to severe cases.
Biologic therapies: These advanced treatments target specific pathways involved in inflammation, such as tumor necrosis factor (TNF) inhibitors like infliximab and adalimumab, especially when conventional treatments are ineffective.
Surgical Intervention: As a last resort, removal of the colon might be necessary to address complications such as severe bleeding, perforation, or toxic megacolon. Surgery can be curative, removing the source of inflammation entirely.
Hospital-Based Management
In cases where severe symptoms manifest, hospital care becomes crucial. Symptoms like persistent high fever, significant blood loss leading to anemia, excessive dehydration, or electrolyte imbalance require close medical supervision. Intravenous fluids and electrolyte replacement are vital to stabilize the patient. Antibiotics may be administered if infection complicates the condition. Post-hospitalization, ongoing follow-up with healthcare providers is essential; regular monitoring every six months helps detect any signs of relapse or complications early.
Skilled management may enable some patients to handle minor flare-ups independently with medication and lifestyle adjustments, but escalation to medical consultation is necessary when symptoms worsen or persist. The prognosis for ulcerative colitis varies, with many individuals achieving remission with proper treatment. Nonetheless, chronic management is key to preventing long-term complications like colon scarring or increased cancer risk.
Living with ulcerative colitis entails adopting a comprehensive approach—integrating medical therapy, dietary regulation, stress management, and regular healthcare visits. Advances in treatment options continue to improve quality of life for affected individuals, emphasizing the importance of personalized care plans tailored to each patient’s needs.