Comprehensive Insights into How Hepatitis C Affects Liver Health and Long-term Outcomes
This comprehensive article explores the effects of hepatitis C on liver health, its progression from infection to cirrhosis, and the advances in treatment options. It emphasizes the importance of early detection, lifestyle modifications, and medical management in preventing severe liver damage and improving patient outcomes. An essential guide for those at risk and healthcare providers alike, highlighting the significance of ongoing monitoring and modern antiviral therapies.
Understanding the Impact of Hepatitis C on Liver Function and Overall Well-being
Hepatitis C is a significant viral infection that primarily targets the liver, one of the body's vital organs responsible for detoxification, metabolism, and nutrient processing. This infection is caused by the hepatitis C virus (HCV), which can lead to a range of health problems if not diagnosed and managed promptly. Understanding how hepatitis C affects the liver, its progression, and potential complications is crucial for patients, healthcare providers, and those at risk.
Hepatitis C infection occurs in two main stages: the acute phase and the chronic phase. The acute phase happens shortly after exposure to the virus and may last for a few weeks to months. During this period, some individuals may experience symptoms such as fatigue, jaundice, fever, or abdominal discomfort, but many remain asymptomatic. A remarkable proportion of those infected—approximately 15%—are able to clear the virus naturally without treatment during this initial period. However, the remaining 85% of individuals develop chronic hepatitis C, a persistent infection that can silently damage the liver over years or decades.
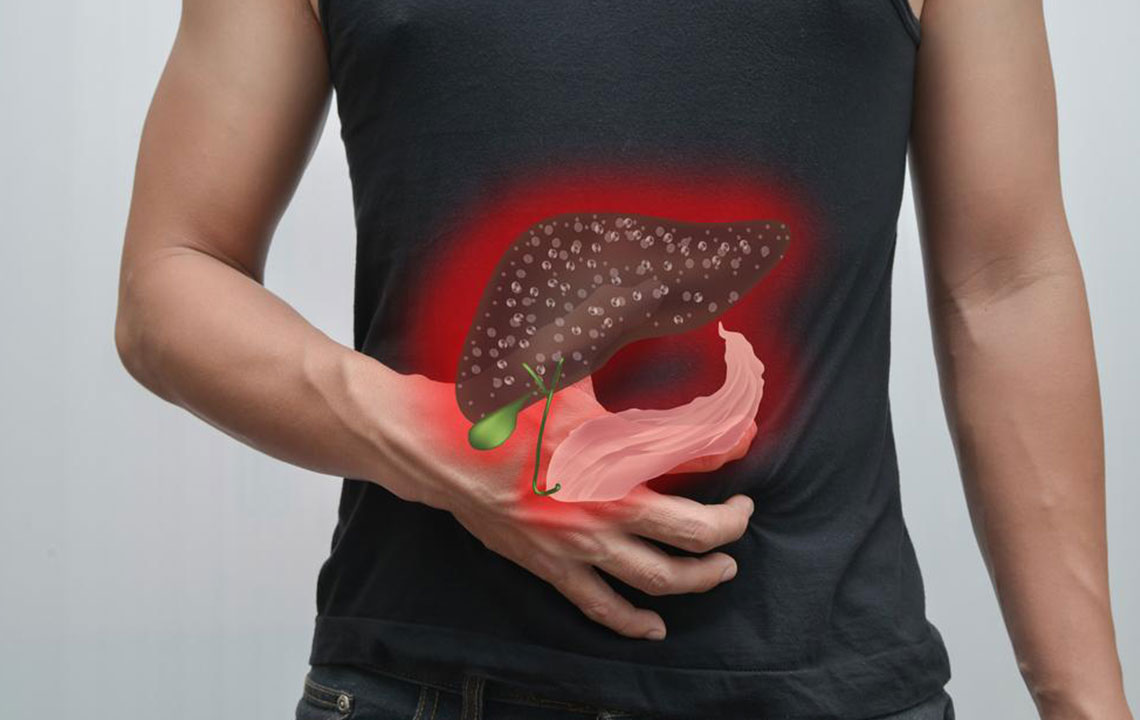
Chronic hepatitis C is often asymptomatic in its early stages, making early diagnosis difficult. Without intervention, the virus gradually causes ongoing inflammation within the liver tissue. This persistent inflammation can lead to the development of scar tissue, a process known as liver fibrosis. Over time, the accumulation of scar tissue significantly impairs the liver's ability to function effectively, a condition called cirrhosis. Cirrhosis can lead to serious complications, including liver failure, portal hypertension, and an increased risk of developing hepatocellular carcinoma, the most common type of liver cancer.
Several factors influence the degree of liver damage caused by hepatitis C. These include the duration of infection, the individual's age at the time of infection, genetic factors, and lifestyle choices such as alcohol consumption. Excess alcohol intake accelerates liver injury, compounding the damage inflicted by the virus. Older age at infection also correlates with faster progression to cirrhosis. Conversely, early detection and treatment can halt or slow disease progression, preserving liver health and improving quality of life.
The advancement of antiviral therapies over recent years has revolutionized hepatitis C management. Direct-acting antivirals (DAAs) now offer highly effective, targeted treatment options that can cure over 95% of cases with a relatively short course of medication. Achieving a sustained virologic response (SVR) through these treatments effectively clears the virus from the body, significantly reducing the risk of cirrhosis and liver cancer. Nevertheless, individuals with longstanding cirrhosis or advanced liver damage require ongoing monitoring, and some may need consideration for liver transplantation.
Patients diagnosed with hepatitis C should undergo regular medical assessments. Routine blood tests, imaging studies, and liver biopsies may be recommended to evaluate the extent of liver damage. Lifestyle modifications, including abstaining from alcohol, maintaining a healthy weight, and managing other health conditions like diabetes, are vital components of comprehensive care. Vaccination against hepatitis A and B viruses is also advised to prevent co-infections that could further compromise liver health.
Public health initiatives and screening programs aimed at high-risk populations have been instrumental in early detection of hepatitis C. Risk groups include individuals who received blood transfusions before blood screening methods improved, intravenous drug users, those with unsterilized tattooing or piercing practices, and specific healthcare workers. Raising awareness about hepatitis C transmission, prevention, and available treatments is essential in controlling and ultimately reducing the prevalence of this silent epidemic.
In summary, hepatitis C poses a significant threat to liver health, with potential progression to cirrhosis and liver cancer if left untreated. Advances in antiviral therapy have made it possible to cure the infection, but early diagnosis and continuous management are key. Adopting a healthy lifestyle, regular medical checkups, and understanding the risks associated with hepatitis C can empower individuals to protect their liver health and avoid severe complications in the future.