Comprehensive Guide to Overactive Bladder: Symptoms, Causes, and Effective Prevention Strategies
This comprehensive guide explores overactive bladder (OAB), detailing its symptoms, causes, risk factors, and management strategies. Understanding the condition early allows for effective treatment, including lifestyle changes, medications, and surgical options. Lifestyle modifications like pelvic exercises and avoiding bladder irritants can significantly reduce symptoms. The article emphasizes the importance of early diagnosis and personalized care to improve quality of life for those affected by OAB.

Comprehensive Guide to Overactive Bladder: Symptoms, Causes, and Effective Prevention Strategies
Overactive bladder (OAB) is a common yet often misunderstood condition characterized by a sudden and uncontrollable urge to urinate, along with frequent urination episodes. This condition significantly impacts quality of life, leading to embarrassment, social withdrawal, and sometimes even emotional distress. Understanding its underlying causes, recognizing symptoms early, and exploring effective management and preventive strategies are crucial for those affected.
Understanding Overactive Bladder: An Overview
Overactive bladder is primarily caused by involuntary contractions of the bladder’s detrusor muscle, which is responsible for storing urine. These spasmodic contractions occur regardless of the volume of urine in the bladder, leading to urgent needs for urination. The condition can be classified into different types depending on the presence or absence of urinary leakage, as well as other factors.
Types of Overactive Bladder
Dry OAB: This form involves recurrent sensations of urgency to urinate without any leakage or incontinence. Individuals with dry OAB often experience multiple urgent trips to the bathroom but do not experience accidents.
Wet OAB: Also known as urge incontinence, this type includes both urgency and involuntary leakage of urine. People affected by wet OAB often face the challenge of managing both the urgency and the risk of accidents.
The underlying mechanism involves spasms in the detrusor muscle—the main muscle in the bladder wall responsible for contraction and urine release. These spasms and the impaired nerve signaling that controls them are often attributed to nerve damage or neurodegenerative diseases. Various factors contribute to the development of OAB, making it a multifaceted condition that demands personalized approaches to management.
Conditions such as Parkinson's disease, multiple sclerosis, and benign prostatic hyperplasia (enlarged prostate) are common neurological or structural causes that disrupt normal bladder function. Age remains a significant risk factor; however, OAB is not an inevitable part of aging, and many lifestyle factors can influence its onset and severity.
Additional contributors include lifestyle choices such as excessive weight, smoking, and certain medications that increase urination. Chronic health issues like urinary tract infections (UTIs) and prolonged coughing due to respiratory problems can exacerbate symptoms. It is essential for individuals experiencing symptoms to seek medical advice for accurate diagnosis and appropriate treatment.
Key Risk Factors for Overactive Bladder
Advanced age, particularly beyond 50 years
Obesity, which exerts pressure on the bladder
Smoking, which can impair bladder function and nerve signaling
Dehydration or excessive fluid intake, disrupting normal bladder regulation
Urinary tract infections, leading to inflammation and irritability
Pregnancy and childbirth, affecting pelvic support structures
Chronic coughing and respiratory issues that increase intra-abdominal pressure
Use of certain medications, such as diuretics, that cause increased urination
Statistics indicate that about one in three men and nearly half of women in the United States experience symptoms of overactive bladder at some point. Common signs include the frequent need to urinate, a sudden inability to delay urination, nocturia (frequent urination at night), and leakage episodes. These symptoms can severely impact daily routines, social activities, and emotional well-being.
Addressing overactive bladder requires a comprehensive approach. Early intervention through lifestyle modifications, medical management, and in some cases, surgical options can help improve quality of life and reduce symptom severity.
Effective Management and Prevention Strategies
Stay Hydrated: Maintain a balanced fluid intake. Avoid excessive consumption or dehydration, both of which can irritate the bladder.
Weight Management: Losing excess weight reduces pressure on the bladder and pelvic floor muscles, alleviating symptoms.
Address Constipation: Preventing constipation helps reduce pelvic pressure, which can contribute to bladder issues.
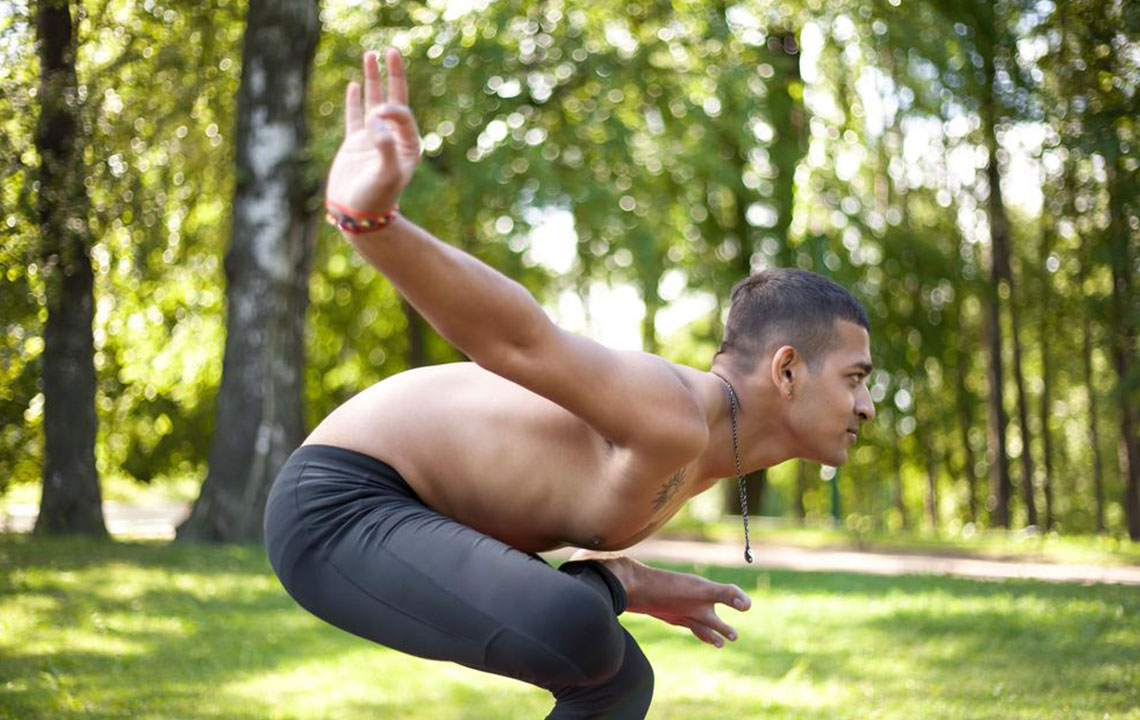
Pelvic Floor Exercises: Engage in Kegel exercises regularly to strengthen bladder-supporting muscles, improving control and reducing leakage.
Prompt Infection Treatment: Seek medical attention for urinary tract infections to prevent the worsening of symptoms and protect bladder health.
Quit Smoking: Smoking damages bladder tissues and impairs nerve signals critical for normal function.
Regular Physical Activity: Exercise supports overall health, improves pelvic muscle tone, and can alleviate symptoms.
Avoid Bladder Irritants: Limit caffeine, spicy foods, acidic fruits, and salty snacks that can irritate the bladder lining and exacerbate urgency.
In addition to lifestyle changes, several medical options are available. These include medications such as antimuscarinics and beta-3 adrenergic agonists designed to relax the bladder muscle. In resistant cases, therapies like nerve stimulation or surgical interventions may be considered. Consulting a healthcare professional enables personalized treatment planning, ensuring effective management.
Living with overactive bladder can be challenging, but with proper diagnosis, lifestyle modifications, and medical treatment, most individuals can effectively control symptoms and regain confidence in daily activities.