Comprehensive Guide to Spinal Degeneration: Understanding Disc and Joint Disorders
This comprehensive article explores spinal degeneration, focusing on degenerative disc disease and degenerative joint disease. It explains their causes, symptoms, differences, and treatment options, highlighting the importance of early diagnosis and management for maintaining spinal health and improving quality of life. Learn how aging impacts your spine and what preventive measures can slow down degeneration.
Comprehensive Guide to Spinal Degeneration: Understanding Disc and Joint Disorders
As we age, various degenerative processes inevitably impact our body tissues, particularly the spine, leading to a range of health issues known collectively as degenerative spinal conditions. These conditions develop gradually over time and are primarily caused by the natural aging process, compounded by lifestyle factors, genetic predisposition, and mechanical stress. Understanding the nuances of spinal degeneration is essential for early detection, effective management, and improved quality of life. This comprehensive guide delves into the core aspects of spinal degeneration, focusing on two predominant conditions: degenerative disc disease and degenerative joint disease, highlighting their differences, symptoms, causes, and treatment options.
Degenerative illnesses related to the spine encompass a broad spectrum of disorders that result from the deterioration of spinal components. These include intervertebral discs, facet joints, ligaments, and bone structures. The two conditions most frequently encountered and often misunderstood are degenerative disc disease (DDD) and degenerative joint disease, commonly referred to as osteoarthritis of the spine. Both conditions predominantly affect individuals as they age but vary considerably in terms of pathology, clinical presentation, and management strategies.
Understanding Degenerative Disc Disease
Degenerative disc disease is a condition characterized by the progressive deterioration of the intervertebral discs — the cushion-like structures situated between the vertebrae. These discs are essential for providing flexibility, absorbing shock, and enabling smooth movement of the spine. Over time, due to aging and repetitive stress, these discs lose their hydration and elasticity, leading to structural changes such as disc thinning, tears, or herniation.
Healthy discs function effectively as shock absorbers, but as they degenerate, their capacity diminishes, which can result in pain, stiffness, and reduced mobility. The loss of disc height can lead to nerve root compression, causing radiating pain, numbness, or weakness in the limbs. Moreover, degenerative disc disease is often associated with other spinal conditions, compounding symptoms and complicating treatment.
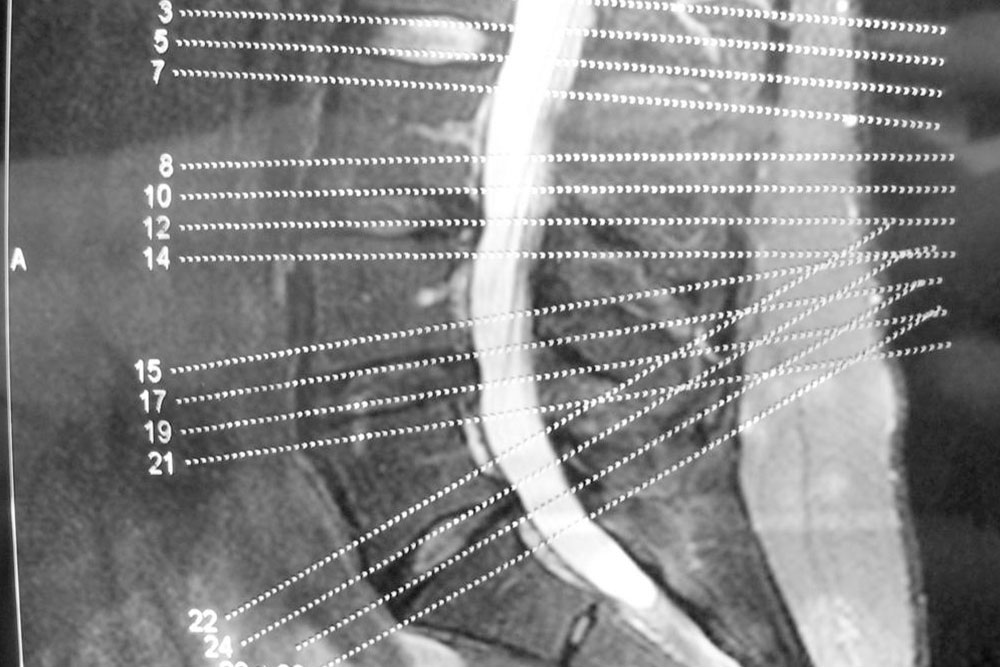
Common causes of degenerative disc disease include aging, genetic predisposition, biomechanical stress from repetitive motions or poor posture, obesity, smoking, and trauma. Symptoms vary widely but often include persistent or intermittent back pain, pain radiating down the legs or arms, and a sensation of stiffness. Diagnosis is typically made through imaging techniques such as MRI, which can reveal disc dehydration, tears, or herniation.
Understanding Degenerative Joint Disease
Degenerative joint disease, or osteoarthritis of the spine, primarily affects the facet joints – small joints located at the back of each vertebra that facilitate movement and stability. These joints are covered with cartilage that allows for smooth, pain-free motion. As aging progresses or due to injury, this cartilage gradually wears away, leading to bone-on-bone contact, inflammation, and pain.
Unlike degenerative disc disease, which affects the cushioning discs, degenerative joint disease results in joint stiffness, swelling, and discomfort. The breakdown of cartilage causes the bones to rub against each other, often resulting in osteophyte formation (bone spurs) that further restrict movement and precipitate pain. This condition can also lead to decreased flexibility in the spine, muscle spasms, and nerve compression if bone spurs impinge on nerves.
The primary factors contributing to degenerative joint disease include age, joint injury, repetitive stress, obesity, and genetic factors. Symptoms often include localized pain, stiffness after periods of inactivity, and decreased range of motion. Diagnosis involves physical examination, X-rays, and MRI scans to assess cartilage loss, bone changes, and joint inflammation.
Key Differences Between the Conditions
While degenerative disc disease and degenerative joint disease both involve age-related deterioration of spinal structures, they differ significantly in their pathology, clinical presentation, and treatment approaches:
Location: DDD affects the discs; degenerative joint disease affects facet joints.
Symptoms: DDD often causes pain that radiates down limbs and may involve nerve compression; osteoarthritis predominantly causes localized pain and stiffness.
Progression: Both are chronic, progressive conditions, but their symptoms and complications evolve differently over time.
Imaging Findings: DDD shows disc dehydration, tears, or herniation; degenerative joint disease reveals cartilage loss, joint narrowing, and bone spurs.
Management and Treatment Options
Effective management of spinal degeneration relies on accurate diagnosis and a comprehensive treatment plan tailored to the individual. Treatment modalities include both conservative and surgical options:
Conservative Treatments: Physical therapy, pain management with NSAIDs or analgesics, activity modification, and lifestyle changes such as weight loss and quitting smoking.
Interventional Procedures: Corticosteroid injections, nerve blocks, or epidural injections to reduce inflammation and relieve pain.
Surgical Options: In cases where conservative treatments fail, procedures such as discectomy, spinal fusion, or artificial disc replacement may be considered.
Prevention strategies focus on maintaining spinal health through regular exercise, proper posture, ergonomic practices, and managing risk factors like obesity and smoking. Early diagnosis and intervention can significantly slow disease progression and improve functional outcomes.
Understanding these conditions—distinguishing between degenerative disc disease and degenerative joint disease—is crucial for effective treatment and improving patients' quality of life. Advances in imaging and minimally invasive surgical techniques continue to enhance outcomes, offering hope for those affected by spinal degeneration.





