In-Depth Overview of the 10 Major Types of Leukemia: Symptoms, Causes, and Treatments
This comprehensive guide explores the ten main types of leukemia, detailing their origins, symptoms, diagnostic methods, and current treatments. By understanding these variants, patients and caregivers can better navigate diagnosis and management options for this complex group of blood cancers. Advances in targeted therapies have improved prognosis, and early detection is critical for effective treatment success.

A Comprehensive Examination of the Top 10 Leukemia Variants
Leukemia is a complex form of blood cancer that originates in the bone marrow, the soft tissue inside bones responsible for producing blood cells. This disease entails the abnormal proliferation of specific blood cells, which can interfere with the body's ability to fight infections, control bleeding, and carry oxygen throughout the body. Understanding leukemias is crucial for early diagnosis and effective treatment.
Leukemia manifests in various forms, classified primarily based on the type of blood cells affected—lymphocytes or myeloid cells—and the speed of progression, either acute or chronic. These distinctions lead to the identification of ten main types, each with unique features, prognosis, and treatment approaches. Here, we delve into each of these ten types, exploring their causes, symptoms, diagnostic methods, and current treatment options to provide a comprehensive guide for patients, families, and healthcare professionals.
1. Acute Lymphoblastic Leukemia (ALL)
ALL is an aggressive form of leukemia originating from immature lymphoid stem cells in the bone marrow. It often progresses rapidly, requiring prompt diagnosis and treatment. It can spread beyond the marrow to the central nervous system, lymph nodes, or testes, making it more complex to treat. This type predominantly affects children, but adults can also be diagnosed, particularly over age 50.
Causes and Risk Factors: Though the exact cause is unknown, genetic mutations and exposure to radiation or certain chemicals may increase risk. Some studies have linked ALL to prior chemotherapy or radiation therapy treatments and familial genetic syndromes.
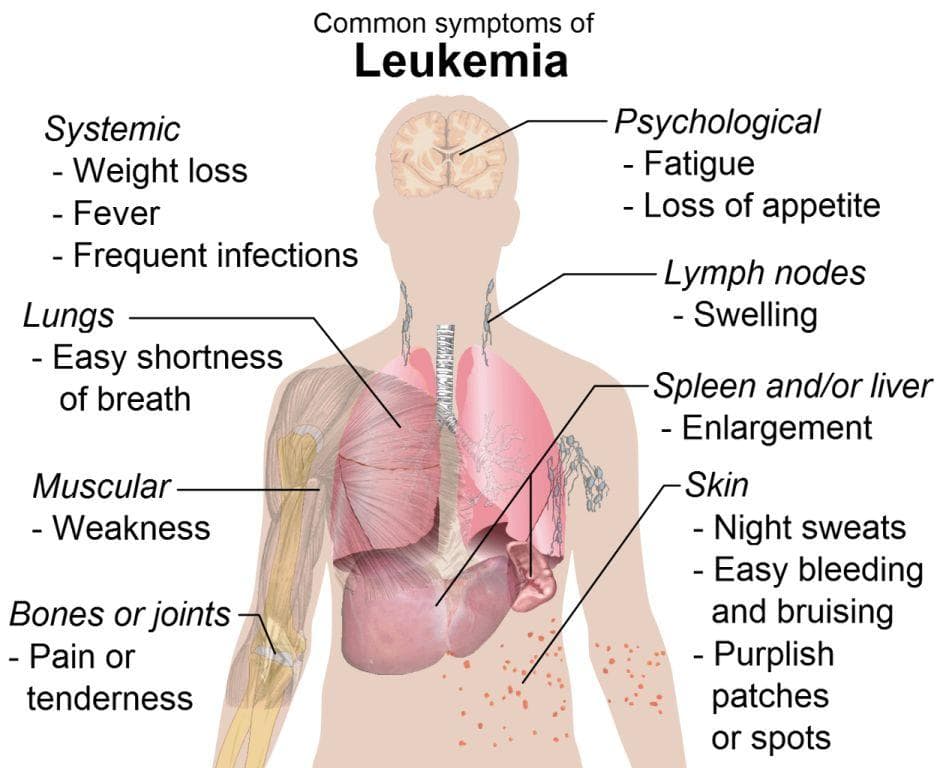
Symptoms: Fatigue, unexpected infections, fever, easy bruising or bleeding, swollen lymph nodes, unexplained weight loss, and bone or joint pain are typical symptoms.
Diagnosis and Treatment: Diagnosis involves blood tests, bone marrow biopsies, and lumbar punctures. Treatment typically includes intensive chemotherapy, targeted therapy, and, in some cases, stem cell transplant. Advances in immunotherapy have improved outcomes significantly.
2. Acute Myeloid Leukemia (AML)
AML arises from mutations in myeloid stem cells, affecting multiple blood components, including red blood cells, white blood cells, and platelets. It progresses rapidly and predominantly affects adults but can also occur in children. AML is characterized by the accumulation of abnormal myeloblasts, which hinder normal blood cell production.
Causes and Risk Factors: Exposure to chemotherapy, radiation, certain chemicals like benzene, smoking, and prior blood disorders increase risk. Genetic mutations and familial predisposition can also play a role.
Symptoms: Symptoms include fatigue, susceptibility to infections, bleeding gums, easy bruising, shortness of breath, and fever.
Diagnosis and Treatment: Similar to ALL, diagnosis involves blood tests, bone marrow examinations, and cytogenetic analysis. Treatment includes intensive chemotherapy, targeted drugs like FLT3 inhibitors, and stem cell transplant. The prognosis depends on age, genetic factors, and response to treatment.
3. Chronic Lymphocytic Leukemia (CLL)
CLL is a slow-growing leukemia primarily affecting older adults, generally those over 60 years old. It involves the accumulation of abnormal, mature-looking lymphocytes that do not function properly. CLL often progresses gradually, with many patients remaining asymptomatic for years and diagnosed incidentally through routine blood work.
Causes and Risk Factors: While the exact cause remains unclear, environmental exposures, genetic factors, and hereditary predisposition play roles. A notable link has been observed between CLL and prolonged exposure to herbicides like Agent Orange.
Symptoms: Fatigue, swollen lymph nodes, weight loss, frequent infections, and easy bruising are common symptoms. Some patients may develop enlarged spleen or liver.
Diagnosis and Treatment: Blood tests, flow cytometry, and bone marrow biopsies determine CLL. Many cases are monitored without treatment initially; when needed, options include chemoimmunotherapy, targeted agents (like BTK inhibitors), and supportive care. Advances in targeted therapies have improved life expectancy for CLL patients.
4. Hairy Cell Leukemia (HCL)
HCL is a rare, slow-growing B-cell malignancy characterized by distinctive hairy projections on the surface of affected lymphocytes. It primarily involves the bone marrow, liver, and spleen, often leading to enlarged spleen and pancytopenia (reduction in red cells, white cells, and platelets). Despite its rarity, HCL generally responds well to treatment, allowing patients to maintain a good quality of life.
Causes and Risk Factors: The origin of HCL remains poorly understood, though environmental exposures and genetic predispositions may contribute.
Symptoms: Fatigue due to anemia, infections from neutropenia, easy bruising, and splenomegaly are typical symptoms.
Diagnosis and Treatment: Diagnosis relies on blood smears, bone marrow biopsy, and immunophenotyping. Treatment options include purine analogs like cladribine or pentostatin, which often induce complete remission. Targeted therapies and biological agents are also under investigation.
5. Chronic Myelomonocytic Leukemia (CMML)
CMML is an uncommon type that manifests as a hybrid between myelodysplastic and myeloproliferative disorders. It involves the proliferation of monocytes—white blood cells that play critical roles in immune response. CMML significantly impairs immune function and often causes symptoms related to anemia, bleeding, or infections.
Causes and Risk Factors: Exposure to environmental toxins, previous chemotherapy, or radiation increases the risk. Genetic mutations are also involved.
Symptoms: Fatigue, fever, night sweats, bleeding tendencies, infections, and enlarged spleen are frequent symptoms.
Diagnosis and Treatment: Blood tests and bone marrow analysis are used for diagnosis. Treatment includes hypomethylating agents, supportive care, and stem cell transplants in eligible patients. The outlook varies based on disease progression and response to therapy.
6. Juvenile Myelomonocytic Leukemia (JMML)
JMML predominantly affects children under the age of five and is marked by uncontrolled growth of monocytes. It is a rare but serious disease that impairs immune function and leads to anemia, infections, and bleeding complications. Often linked to genetic mutations, JMML requires prompt diagnosis for effective management.
Causes and Risk Factors: Genetic mutations in the RAS pathway are common. Family history and early developmental issues may contribute.
Symptoms: Fever, failure to thrive, enlarged liver and spleen, anemia, and bleeding tendencies.
Diagnosis and Treatment: Blood tests, genetic analyses, and bone marrow examination are essential. Bone marrow transplantation is currently the most promising treatment, offering potential cure. Supportive care helps manage symptoms while definitive treatment is pursued.
7. Large Granular Lymphocytic Leukemia (LGL)
LGL is a chronic leukemia primarily affecting middle-aged adults and involves the proliferation of large granular lymphocytes—T cells or natural killer (NK) cells. It often presents with an enlarged spleen and liver along with mild symptoms. While generally indolent, LGL can cause cytopenias and complications from immune dysregulation.
Causes and Risk Factors: Chronic infections or autoimmune disorders can predispose individuals to LGL. Genetic factors may also play a role.
Symptoms: Fatigue, low blood counts, splenomegaly, and occasional infections.
Diagnosis and Treatment: Diagnosis involves blood smears, immunophenotyping, and spleen imaging. Management may include immunosuppressive therapy or watchful waiting, depending on severity.
8. Blastic Plasmacytoid Dendritic Cell Neoplasm
Recognized by WHO as related to AML, this is a very rare leukemia primarily affecting white blood cells, spleen, and platelets. It can involve lymph nodes but often presents with subtle symptoms, making diagnosis challenging. This form tends to be aggressive, requiring intensive treatment.
Causes and Risk Factors: The disease mechanisms are not entirely understood, but chromosomal abnormalities may contribute.
Symptoms: Lymphadenopathy, fevers, skin rashes, and fatigue are typical but often nonspecific.
Diagnosis and Treatment: Diagnosis involves specialized immunohistochemistry and genetic testing. Treatment often includes chemotherapy regimens similar to AML and stem cell transplant, with ongoing research into targeted therapies.
9. B-cell Prolymphocytic Leukemia (B-PLL)
B-PLL is an aggressive B-cell leukemia usually diagnosed around age 70. It results from excessive growth of lymphocytes, affecting spleen, liver, and lymph nodes. It often presents with high white blood cell counts, anemia, and bleeding tendencies.
Causes and Risk Factors: Genetic mutations and chromosomal abnormalities are involved, with a higher incidence in elderly males.
Symptoms: Splenomegaly, weight loss, night sweats, anemia, and bleeding issues often characterize B-PLL.
Diagnosis and Treatment: Blood tests, bone marrow biopsies, and flow cytometry assist in diagnosis. Treatment options include chemotherapy, targeted therapies, and stem cell transplantation, though prognosis remains guarded.
10. T-cell Prolymphocytic Leukemia (T-PLL)
This is an extremely rare and aggressive leukemia affecting T-lymphocytes, primarily in older men. Often linked to chromosomal abnormalities, T-PLL causes rapid disease progression with symptoms like lymphadenopathy, hepatosplenomegaly, skin lesions, and cytopenias. Without treatment, multi-organ failure can occur.
Causes and Risk Factors: Chromosomal mutations and immune dysregulation are common factors.
Symptoms: Swollen lymph nodes, enlarged spleen and liver, skin rashes, and anemia.
Diagnosis and Treatment: Diagnosed through immunophenotyping, genetic analysis, and imaging. Treatment may include aggressive chemotherapy, monoclonal antibodies, and stem cell transplantation. Despite intensive therapy, T-PLL remains challenging to treat effectively.