Comprehensive Guide to Recognizing and Managing Overactive Bladder Symptoms
Overactive bladder (OAB) impacts millions worldwide, causing urgent need to urinate, frequent trips to the bathroom, and night-time disruptions. Recognizing symptoms early is key to managing this condition effectively. This detailed guide explores the signs, causes, risk factors, and treatment options for OAB, emphasizing the importance of prompt medical consultation. With lifestyle adjustments, medications, and advanced therapies, individuals can significantly improve their quality of life, reduce symptoms, and regain control over their urinary health. Learn how to identify and address OAB symptoms today.

Understanding the Key Symptoms and Indicators of Overactive Bladder (OAB)
Overactive bladder (OAB) is a common urological condition that affects millions of people worldwide. Characterized by a sudden and uncontrollable urge to urinate, OAB can significantly disrupt daily routines and diminish quality of life. Despite its prevalence, many individuals remain unaware of the symptoms or delay seeking medical advice. In this comprehensive guide, we explore the various indicators of overactive bladder, including signs, causes, risk factors, and effective management strategies to improve health outcomes.
Overactive bladder manifests primarily through a set of recognizable symptoms that can vary in intensity among individuals. The most prominent feature is a sudden, intense urge to urinate that occurs unexpectedly and often without warning. This urgency can make it challenging to reach the bathroom in time, leading to involuntary urine leakage or accidents. Many sufferers experience frequent urination—more than eight times within a 24-hour period—even when the bladder isn't full. Such heightened urinary frequency can interfere with daily activities, work, and social interactions.
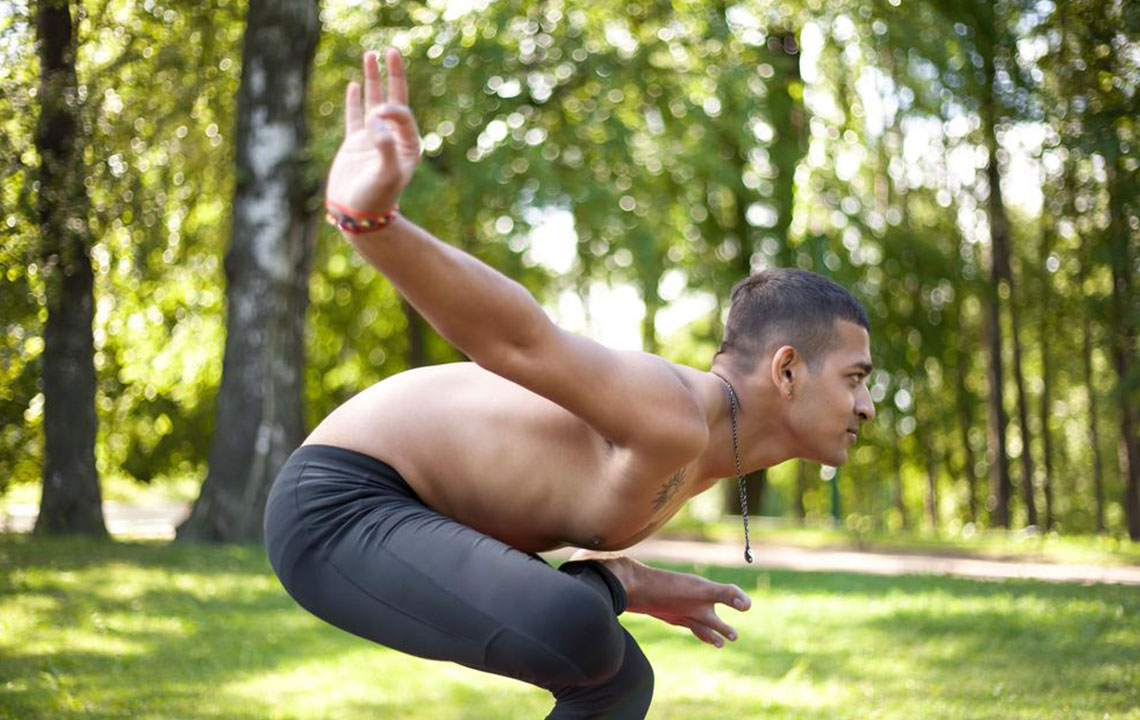
Besides urgency and frequency, nocturia—waking up multiple times during the night to urinate—is a common symptom associated with OAB. Nocturia not only disturbs sleep but also contributes to daytime fatigue, decreased concentration, and overall declining health. Urinary incontinence, especially during physical exertion like running or jumping, is another typical indicator and can be distressing psychologically, causing embarrassment or social withdrawal.
Monitoring persistent nocturia over several nights, particularly when combined with other symptoms, can hint at underlying overactive bladder issues. It’s essential to seek medical evaluation if these signs persist, as early diagnosis and intervention can improve management outcomes. Healthcare professionals can recommend lifestyle modifications, behavioral therapies, medications, or other treatments tailored to individual needs.
Age plays a crucial role in the development of OAB. As individuals grow older, muscle tone and bladder capacity tend to decline, increasing susceptibility to symptoms. Women are particularly prone to OAB due to the physiological changes caused by pregnancy, childbirth, and menopause, which can weaken bladder muscles and alter pelvic floor support. In men, prostate enlargement remains a significant factor contributing to urinary symptoms akin to OAB.
Furthermore, various medical conditions can heighten the risk of developing overactive bladder. These include neurological disorders such as Parkinson’s disease, multiple sclerosis, or spinal cord injuries, which impair nerve signals responsible for bladder control. Chronic illnesses such as diabetes and strokes can also damage nerves or affect bladder function. Obesity, which increases abdominal pressure, can strain bladder muscles, exacerbating symptoms. Other health issues influencing OAB include urinary tract infections, prostate problems in men, tumors, and dementia.
Understanding these risk factors underscores the importance of early detection and comprehensive management of overactive bladder. Individuals experiencing symptoms should consult healthcare providers promptly to identify causes and develop personalized treatment plans. Managing OAB effectively can alleviate symptoms, reduce psychological stress, and restore mobility and independence.
In addition to medical treatments, adopting lifestyle changes such as pelvic floor exercises, dietary modifications, fluid management, and bladder training can significantly reduce symptoms. Medications like anticholinergics and beta-3 adrenergic agonists are commonly prescribed to help control urgency and leakage. For some, minimally invasive procedures or surgical options may offer relief when conservative treatments fail.
In conclusion, recognizing the signs and symptoms of overactive bladder early can lead to improved quality of life. With advances in medical science and a better understanding of underlying causes, individuals affected by OAB now have access to a range of effective management strategies. If you experience frequent urination, sudden urges, nocturia, or involuntary leaks, consult a healthcare professional to explore diagnosis and tailored treatment options that meet your needs and help restore your comfort and confidence.