Comprehensive Natural Approaches to Lower Blood Sugar Levels Effectively
Learn comprehensive natural strategies and lifestyle modifications to effectively lower blood sugar levels. This detailed guide covers understanding blood sugar, monitoring methods, diet, exercise, and when to seek medical advice, empowering you to manage your condition proactively and prevent diabetes-related complications.

Comprehensive Natural Approaches to Lower Blood Sugar Levels Effectively
Elevated blood sugar levels, if left unmanaged, pose significant health risks, including the development of chronic diseases such as diabetes. Achieving and maintaining optimal blood glucose levels is vital for overall health and well-being. Understanding the intricate mechanisms of blood sugar regulation and the factors influencing it can empower individuals to take proactive steps toward better management. This article provides an in-depth exploration of natural strategies, lifestyle modifications, and essential knowledge about blood sugar management to help you maintain healthy levels and prevent complications.
Blood sugar, also known as blood glucose, originates from the carbohydrates we consume. The pancreas plays a central role in regulating blood glucose by secreting insulin, a hormone responsible for facilitating the uptake of glucose into cells for energy or storage. When insulin production diminishes or the body's cells become resistant to insulin's effects, blood glucose levels rise abnormally, culminating in diabetes. Understanding this process is fundamental to developing effective strategies for managing blood sugar naturally.
Understanding Types of Diabetes and Their Impact
Diabetes manifests primarily in three forms: Type 1, Type 2, and gestational diabetes. Type 1 diabetes is an autoimmune condition where the body's immune system attacks insulin-producing cells in the pancreas, necessitating lifelong insulin therapy. Type 2 diabetes, accounting for approximately 90% of cases worldwide, results from insulin resistance combined with inadequate insulin production. Gestational diabetes occurs during pregnancy and requires specific management to protect maternal and fetal health. The focus of this article is predominantly on Type 2 diabetes, which is closely linked to lifestyle factors and can often be effectively managed with natural interventions.
What Are Normal Blood Sugar Levels?
Maintaining blood sugar within a healthy range is crucial for preventing long-term health issues. Typically, a fasting blood sugar level between 70-99 mg/dL is considered normal. Post-meal, blood sugar should be below 140 mg/dL when measured two hours after eating. Readings consistently exceeding 126 mg/dL during fasting or 200 mg/dL randomly suggest abnormal glucose regulation and warrant medical consultation. Regular monitoring helps detect fluctuations early, allowing for timely interventions.
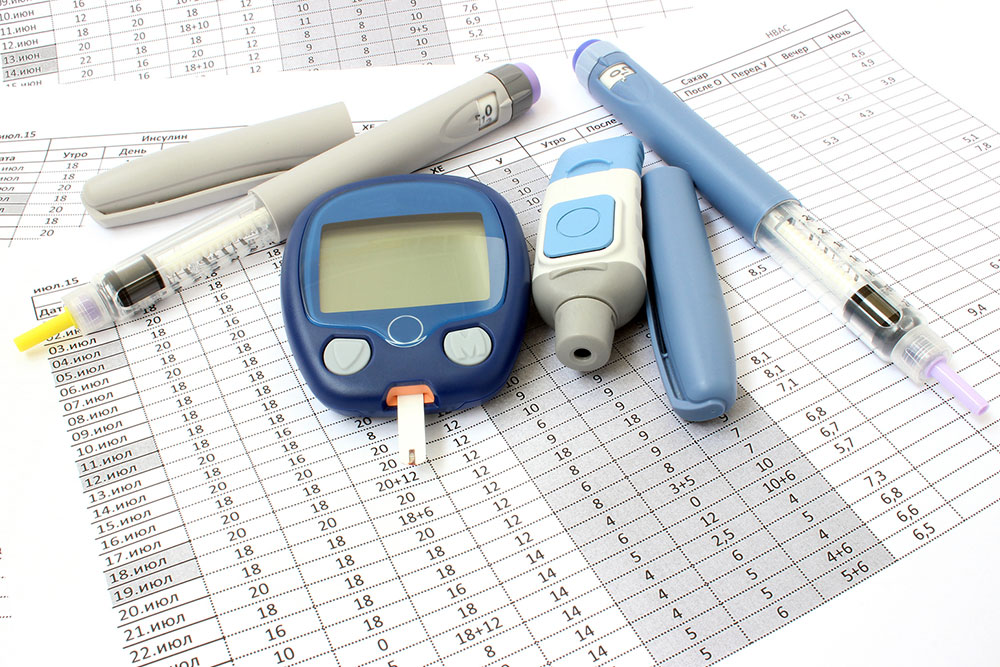
Methods for Blood Sugar Monitoring
Accurate assessment of blood sugar levels is essential for effective management. Common tests include the HbA1c test, which reflects the average blood glucose over the past 2-3 months, providing insights into long-term control. Fasting plasma glucose (FPG) tests require fasting for 8-12 hours, offering a snapshot of basal blood sugar. Oral glucose tolerance tests (OGTT) evaluate the body's response to a glucose load. Regular testing using these methods enables individuals to keep track of their condition, adjust lifestyle habits, and work closely with healthcare providers to prevent the progression of diabetes and its associated complications, such as cardiovascular disease, kidney damage, and nerve impairment.
Natural and Lifestyle Strategies to Lower Blood Sugar
Achieving optimal blood sugar levels naturally involves consistent lifestyle modifications alongside medical guidance. Several evidence-based strategies can significantly influence blood glucose control:
Effective Weight Management – Excess weight, especially abdominal fat, contributes to insulin resistance. Implementing gradual, sustained weight loss through balanced diet and exercise can markedly reduce blood sugar levels and improve overall metabolic health. Even a modest reduction of 5-10% of body weight can produce substantial benefits.
Regular Physical Activity – Engaging in at least 150 minutes of moderate-intensity aerobic activity weekly, such as brisk walking, cycling, or swimming, enhances insulin sensitivity. Incorporating strength training exercises twice a week supports muscle mass, further aiding glucose utilization.
Healthy Diet Choices and Lifestyle Habits – Emphasize a diet rich in fiber, lean proteins, healthy fats, and low-glycemic index foods. Reduce intake of refined carbohydrates, sugary snacks, and processed foods. Limit alcohol consumption, as excessive intake can cause blood sugar spikes and interfere with liver function. Prioritize balanced meals with adequate vegetables, nuts, seeds, and whole grains to stabilize blood glucose.
Meditation and Stress Reduction – Chronic stress impacts hormone levels, including cortisol, which can elevate blood sugar. Practices such as yoga, meditation, deep breathing exercises, and adequate sleep support hormonal balance and improve insulin effectiveness.
Hydration and Natural Supplements – Staying well-hydrated with water helps dilute blood sugar levels and supports kidney function. Some natural supplements like fenugreek, chromium, cinnamon, and alpha-lipoic acid have shown promising results in glucose regulation; however, consult a healthcare professional before use.
Role of Medication and When to Seek Medical Advice
While lifestyle modifications form the foundation of managing blood sugar naturally, some individuals may require medication or insulin therapy, especially in advanced cases. Medications such as Metformin, insulin injections, and other oral hypoglycemics are prescribed based on individual health assessment. Regular check-ups are vital to monitor progress, adjust treatments, and prevent complications.
Managing blood sugar levels can be complex, particularly during episodes of hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar). Hyperglycemia (>240 mg/dL) can cause fatigue, blurred vision, and dehydration; it requires dietary adjustments, medication, and exercise. Hypoglycemia (<70 mg/dL) may lead to dizziness, confusion, or loss of consciousness, and demands immediate carbohydrate intake. Always keep glucose tablets or quick-acting carbohydrate sources handy for emergencies. Consistently working with healthcare professionals ensures safe and effective blood sugar management.
In conclusion, adopting natural strategies such as balanced nutrition, regular physical activity, stress management, and proper hydration can significantly improve blood sugar control. Coupled with medical guidance, these practices not only prevent diabetes progression but also enhance overall health. With dedication and informed choices, individuals can lead healthier lives and reduce the risk of long-term complications associated with high blood sugar levels.