Comprehensive Guide to Celiac Disease: Causes, Symptoms, and Management
This comprehensive article explores celiac disease, focusing on its causes, symptoms, diagnosis, and management. It highlights the importance of early detection, proper dietary adherence, and lifestyle adjustments for living healthily with this autoimmune disorder. Whether you are at risk or seeking to understand the disease better, this guide offers detailed insights into celiac disease's complexities and treatment options.
Understanding the Causes, Symptoms, and Treatments of Celiac Disease
Celiac disease, also known as gluten-sensitive enteropathy, is a complex autoimmune disorder that affects millions worldwide. This condition is triggered by the ingestion of gluten, a protein predominantly found in wheat, barley, and rye. For individuals with genetic susceptibility, consuming these grains leads to an abnormal immune response that damages the small intestine's lining, specifically the villi—tiny finger-like projections vital for nutrient absorption. The erosion of villi results in malabsorption, which manifests through a variety of symptoms and health complications.
Understanding the origins of celiac disease involves exploring both genetic and environmental factors. Research indicates that a genetic predisposition plays a crucial role, with certain human leukocyte antigen (HLA) genes, particularly HLA-DQ2 and HLA-DQ8, being strongly associated with the disease. If a family member has celiac disease, the likelihood of developing it increases significantly. However, environmental influences are equally important; high gluten consumption is a primary risk factor, especially in early childhood or in diets rich in gluten-containing foods. Moreover, external factors such as major surgeries, pregnancy, viral infections, and psychological stress can act as triggers, initiating the disease process even in genetically predisposed individuals.
One of the hallmark features of celiac disease is the immune-mediated damage to the intestinal villi. When gluten is consumed, the immune system mistakenly identifies gluten as a harmful substance, producing an attack that damages the small intestinal lining. This damage impairs the intestine's ability to absorb nutrients effectively, leading to a spectrum of clinical manifestations. The most common and immediate symptoms include diarrhea, weight loss, fatigue, and bloating. These symptoms can often be subtle or mistaken for other conditions, making diagnosis challenging without proper testing.
In adults, celiac disease can present with diverse symptoms beyond gastrointestinal issues. Patients might experience anemia due to iron deficiency, osteoporosis resulting from calcium malabsorption, skin rashes such as dermatitis herpetiformis, and persistent acid reflux. Neurological symptoms like headaches, peripheral neuropathy, and cognitive difficulties—sometimes referred to as 'brain fog'—are also reported. Moreover, some adults may develop psychiatric conditions such as depression or anxiety, which can complicate the diagnosis further.
Children with celiac disease often showcase different symptoms. Common signs include chronic diarrhea, abdominal distention, and failure to thrive, which can lead to delayed development if left untreated. Other pediatric symptoms include irritability, poor appetite, and weight loss. Neurological manifestations in children may involve attention deficit hyperactivity disorder (ADHD), learning difficulties, or seizures, underscoring the systemic impact of the disease.
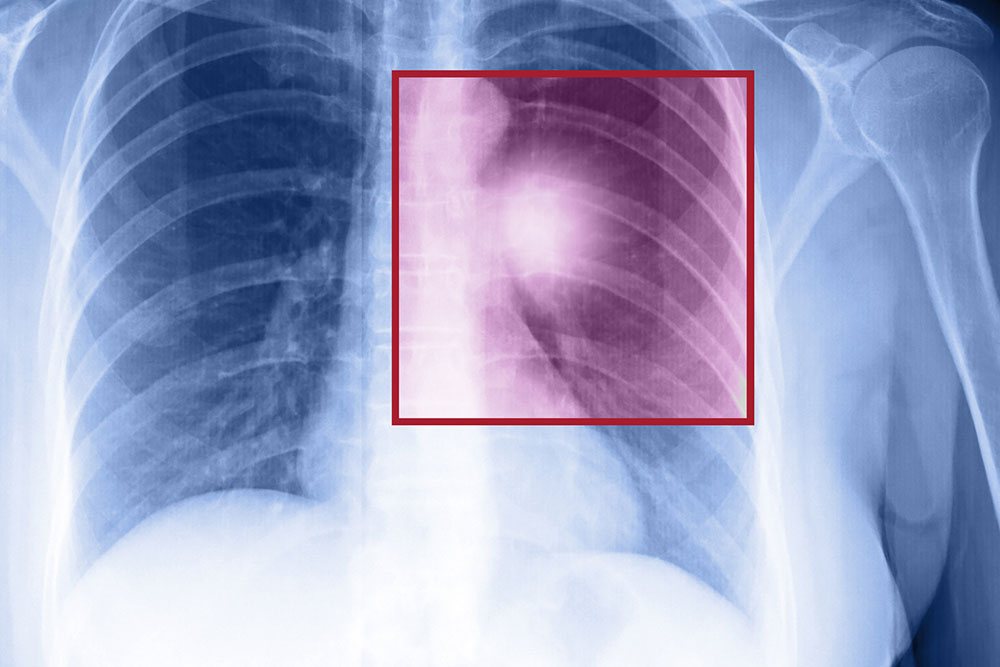
Diagnosis of celiac disease involves a combination of clinical evaluation, serological testing, and confirmatory intestinal biopsy. Blood tests for anti-tissue transglutaminase antibodies (tTG-IgA) are typically the first step. If positive, an endoscopic biopsy of the small intestine is performed to assess villous atrophy, which confirms the diagnosis. It's crucial that patients continue consuming gluten during testing to avoid false negatives. Once diagnosed, the cornerstone of treatment is adhering to a strict gluten-free diet, which prevents immune system activation and allows intestinal healing.
Managing celiac disease also involves nutritional counseling, monitoring for deficiencies in iron, calcium, vitamin D, and other nutrients, and addressing associated conditions such as dermatitis herpetiformis or neurological symptoms. Some patients might require medications like steroids or immune suppressants if complications or severe symptoms persist despite dietary adherence. Regular follow-up is essential to monitor intestinal healing and ensure nutritional needs are met.
Living with celiac disease requires comprehensive lifestyle adjustments, including strict avoidance of gluten-containing foods, careful reading of food labels, and awareness of cross-contamination risks. With proper management and ongoing medical support, most individuals can lead healthy, active lives without significant limitations. Advances in gluten detection technology and increased public awareness continue to improve the quality of life for those affected by this autoimmune disorder.
In summary, celiac disease is a multifaceted autoimmune condition with a complex interplay of genetic and environmental factors. Recognizing the symptoms early, obtaining an accurate diagnosis, and adhering to a gluten-free diet are essential steps toward effective management. Continued research and awareness efforts are vital to improve outcomes for patients worldwide.