Comprehensive Guide to Pulmonary Embolism: Recognizing Symptoms and Diagnostic Approaches
This comprehensive article explores pulmonary embolism, emphasizing its symptoms, risk factors, and modern diagnostic techniques. Early detection is vital for effective treatment and improved survival rates. Learn about the latest advancements in PE diagnosis to safeguard your health.

Understanding Pulmonary Embolism: Signs, Symptoms, and Diagnostic Strategies
Pulmonary embolism (PE) is a serious medical condition that arises when a blood clot or other material blocks blood flow in the arteries of the lungs. This potentially life-threatening health issue demands quick recognition and immediate medical intervention. Pulmonary embolism usually results from blood clots that originate elsewhere in the body, such as deep veins in the legs, and travel to the lungs through the bloodstream. The severity of PE can vary from minor discomfort to sudden death, which underscores the importance of understanding its symptoms and diagnostic methods.
Symptoms associated with pulmonary embolism can develop rapidly, often without warning. One of the most common and recognizable signs is sudden, unexplained shortness of breath. Patients may find it difficult to breathe, even during rest, which can be alarming. Chest pain is another typical symptom, often described as sharp and stabbing, which may worsen during deep breaths or coughing. Some individuals might cough up blood, indicating bleeding within the lungs. Rapid heartbeat or tachycardia frequently accompanies PE, reflecting the heart's attempt to compensate for reduced oxygen supply.
Additional symptoms may include dizziness or fainting, a sense of anxiety or impending doom, and swelling or tenderness in the legs if deep vein thrombosis is involved. Recognizing these symptoms early is crucial because pulmonary embolism can escalate quickly, leading to respiratory failure or cardiac arrest if left untreated.
Risk Factors Contributing to Pulmonary Embolism
Several risk factors increase an individual's likelihood of developing PE. Deep vein thrombosis (DVT) is the primary precursor condition, where blood clots form in deep veins, usually in the legs or pelvis. When these clots dislodge, they can travel through the bloodstream and lodge in the lungs.
Prolonged immobility, such as long flights, hospital stays, or bed rest after surgery, can lead to blood stasis and clot formation. Obesity is also a significant risk factor due to increased pressure in veins and reduced mobility. Certain medical conditions, including cancer, heart disease, and inherited blood clotting disorders, further elevate the risk of developing blood clots.
Hormonal therapies, such as oral contraceptives and hormone replacement therapy, are associated with increased clotting risk. Smoking, advanced age, and pregnancy also contribute to a higher susceptibility to pulmonary embolism. Awareness of these risk factors can help in early identification and preventive measures.
Diagnostic Techniques for Pulmonary Embolism
Prompt and accurate diagnosis is essential to managing PE effectively. Medical professionals utilize a combination of clinical evaluation, imaging tests, and blood analyses to confirm the diagnosis.
Physical Examination and Medical History: The initial step involves assessing symptoms, risk factors, and physical signs such as leg swelling or tenderness.
Blood Tests: D-dimer testing measures a protein fragment that is released when a blood clot dissolves. Elevated levels can suggest the presence of an abnormal clot but are not definitive. Negative D-dimer tests may help rule out PE in low-risk patients.
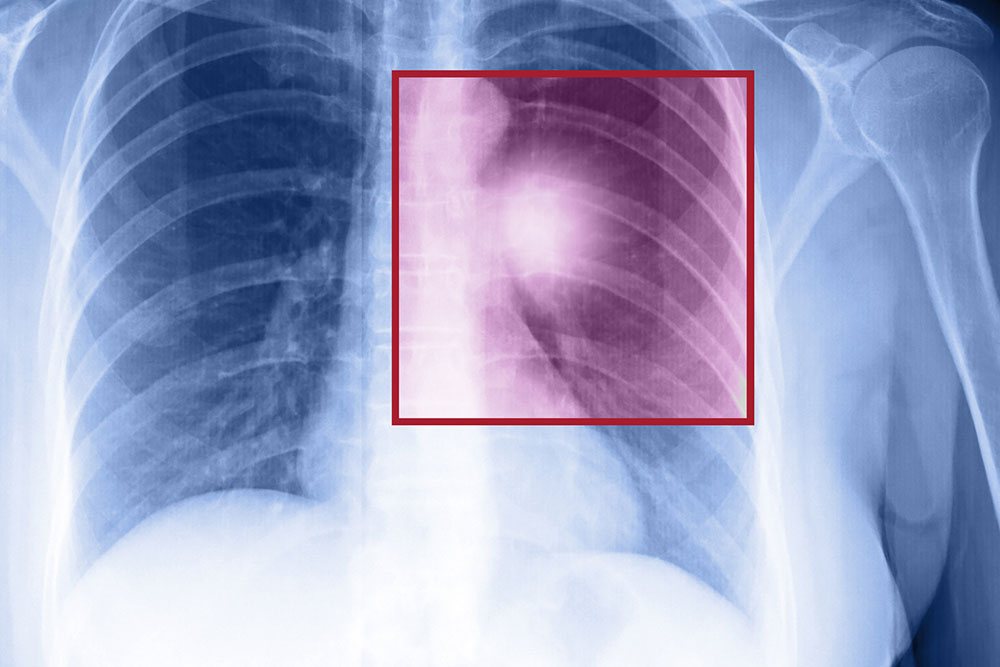
Imaging Studies: The primary imaging modality is the computed tomography pulmonary angiography (CTPA), which provides detailed images of the lung arteries and can directly visualize clots. Chest X-rays are commonly performed but often have nonspecific findings.
V/Q Scan: Ventilation-perfusion scans evaluate airflow and blood flow in the lungs, helping detect blockages when CT scans are contraindicated.
Ultrasound: Doppler ultrasound of the legs can identify DVT, indicating a possible source of emboli.
Advancements in Diagnostic Methods
Recent technological improvements have enhanced the sensitivity and specificity of PE detection. Innovations like multislice CT scanners allow faster image acquisition with higher resolution, reducing diagnostic ambiguity. Additionally, novel blood biomarkers and combined scoring systems improve risk stratification and decision-making processes in acute settings.
Importance of Early Detection and Treatment
Early diagnosis of pulmonary embolism is life-saving. Once diagnosed, immediate treatment aims to prevent clot propagation, reduce the risk of recurrent emboli, and restore normal blood flow. Standard treatment includes anticoagulant medications, such as heparin and warfarin, which thin the blood and prevent new clots from forming. In severe cases, thrombolytic therapy or surgical removal of the clot (embolectomy) may be necessary.
Patients diagnosed with PE require careful monitoring and follow-up to prevent complications like chronic thromboembolic pulmonary hypertension. Educating at-risk populations about symptoms and encouraging prompt medical attention can significantly improve outcomes and survival rates.
In conclusion, pulmonary embolism is a critical condition that demands awareness of its symptoms, risk factors, and diagnostic options. Advances in medical technology have greatly improved our ability to detect PE early, enabling timely treatment and reducing mortality. Recognizing the signs and seeking immediate medical help can make all the difference in saving lives and preventing serious health consequences.