A Comprehensive Guide to Gastrointestinal Stromal Tumors (GIST): Causes, Symptoms, and Treatment Options
Gastrointestinal Stromal Tumors (GIST) are rare tumors originating in the digestive tract's connective tissues, often involving mutations in tyrosine kinase genes like KIT. Early diagnosis through imaging and biopsy is crucial, with treatment typically involving surgical removal and targeted therapies such as TKIs like imatinib. This comprehensive guide covers their causes, symptoms, diagnostic methods, and the latest treatment options, emphasizing the importance of early intervention for better prognosis. Advances in genetics and targeted treatments continue to improve outcomes for GIST patients, highlighting the importance of awareness and timely medical care.

Gastrointestinal Stromal Tumors, commonly known as GISTs, are a type of mesenchymal tumor that originates within the gastrointestinal (GI) tract's connective tissues. These tumors arise when abnormal growth of certain specialized cells occurs, primarily affecting the interstitial cells of Cajal, which are crucial for coordinating gut motility. The development of GISTs is influenced by genetic mutations, most notably those affecting tyrosine kinase enzymes such as KIT and PDGFRA. These mutations lead to uncontrolled cell proliferation, forming tumors that can range from benign to malignant.
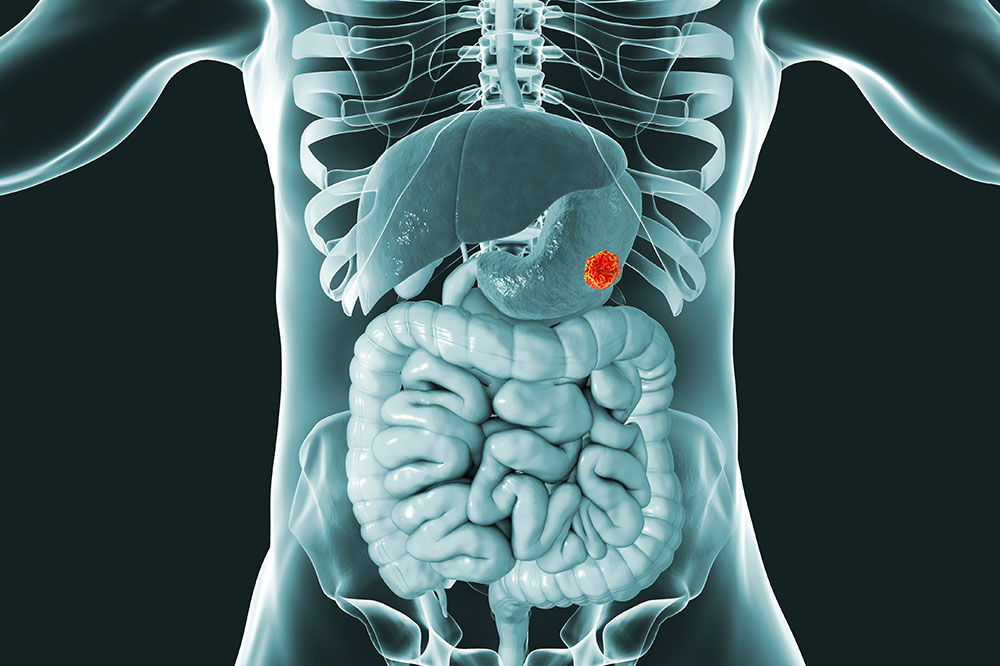
GISTs predominantly develop in the stomach and small intestine but can be found anywhere along the entire length of the GI tract, including the esophagus, colon, and rectum. Although they are relatively rare, accounting for less than 3% of all gastrointestinal cancers, their potential for malignancy makes early detection and effective treatment essential.
The causes of GISTs involve genetic factors, particularly mutations in the KIT gene (most common) and PDGFRA gene. These genetic alterations lead to abnormal activation of tyrosine kinase receptors, which promote cell division and survival, contributing to tumor formation. While most cases occur sporadically, rare familial cases have been identified, indicating a genetic predisposition. Environmental factors have not been conclusively linked to GIST development.
Symptoms of GISTs can be subtle and often go unnoticed for years. Patients may experience abdominal discomfort, pain, or swelling, often mistaken for indigestions or other benign gastrointestinal issues. Other common symptoms include feeling full after eating only small amounts, nausea, vomiting, anemia, and unexplained weight loss. Larger tumors may cause bleeding, leading to blood in the stool, which is a significant concern requiring immediate medical attention.
Diagnosis of GISTs involves a combination of imaging techniques and tissue sampling. Endoscopy, CT scans, MRI, and ultrasound are commonly used to locate and assess the size and extent of the tumor. Confirmatory diagnosis requires a biopsy, where tissue samples are examined histologically. The presence of specific markers, such as CD117 (KIT) and DOG1, helps pathologists distinguish GISTs from other gastrointestinal tumors.
Modern treatment approaches for GISTs are tailored to the tumor's size, location, and whether it has spread. Surgery remains the primary treatment for localized tumors, aiming to remove the tumor entirely with clear margins. Advances in minimally invasive surgical techniques, like laparoscopic procedures, have reduced recovery times and improved patient outcomes.
For tumors that have spread or cannot be surgically removed, targeted drug therapy is the mainstay of treatment. Tyrosine kinase inhibitors (TKIs), such as imatinib (Gleevec), have revolutionized GIST management by specifically targeting mutated kinases involved in tumor growth. These medications can control the disease, shrink tumors, and improve survival rates. In cases of resistance or intolerance to initial therapies, other TKIs like sunitinib and regorafenib may be employed.
Monitoring of GIST patients involves regular imaging and clinical assessments to detect any recurrence or progression. Adjunct therapies, including radiotherapy or chemotherapy, are typically less effective but may be considered in select cases. Supportive care focuses on managing symptoms and improving quality of life.
Advances in molecular genetics and targeted therapies continue to improve the prognosis for patients with GIST. Early detection remains critical to successfully treating these tumors before they pose significant health risks. Public awareness and prompt medical evaluation of persistent gastrointestinal symptoms are essential for timely diagnosis and intervention.