Comprehensive Dietary Guidelines: Essential Foods to Limit When Managing Colitis Effectively
This comprehensive guide offers essential dietary recommendations for managing ulcerative colitis. It highlights foods to limit, including gluten, alcohol, high-fiber foods, sulfates, nuts, dairy, caffeine, spicy foods, and sugary products, to reduce inflammation and control symptoms. Personalized dietary strategies, combined with medical advice, can help improve quality of life and prevent flare-ups. Learn practical tips on selecting suitable foods and avoiding common triggers to effectively manage colitis through diet. An informed approach empowers patients to lead healthier, symptom-free lives.

Critical Dietary Restrictions for Managing Colitis
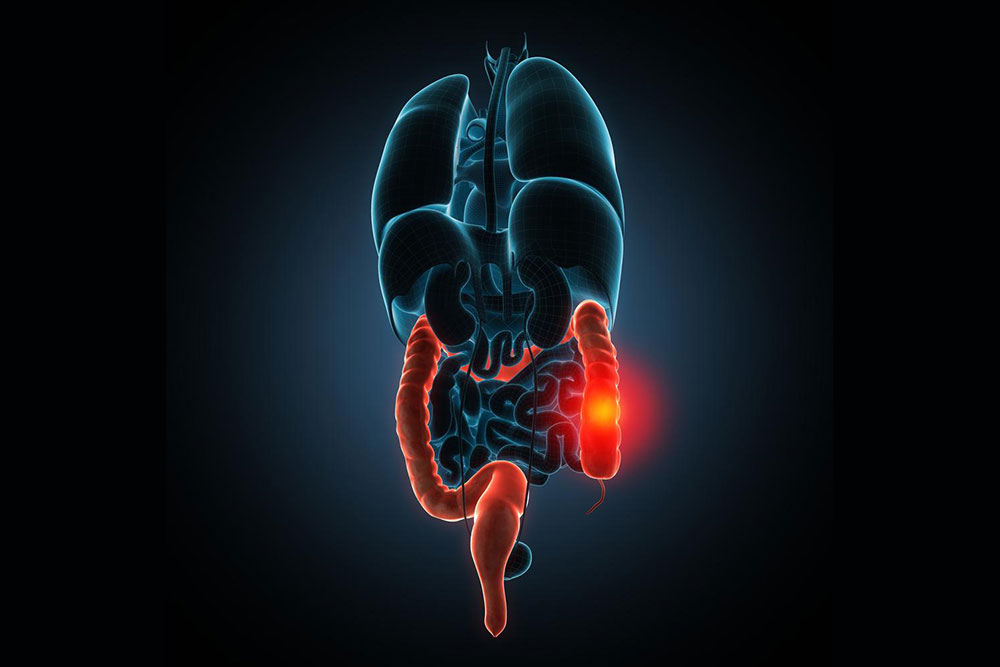
Ulcerative colitis is a persistent, incurable inflammatory bowel disease that targets the lining of the colon and rectum. It manifests through a range of uncomfortable symptoms, including rectal bleeding, persistent abdominal pain, cramping, urgent diarrhea, and fatigue. The severity of flare-ups can vary widely between individuals, and diet plays a significant role in either alleviating or exacerbating these symptoms. Therefore, understanding what foods to limit is crucial for effective disease management. A carefully curated diet that minimizes intake of certain foods can significantly reduce inflammation, improve quality of life, and prevent severe flare-ups.
Central to managing ulcerative colitis is avoiding foods that trigger inflammation, increase gastrointestinal irritation, or cause undesirable symptoms like bloating, gas, and diarrhea. Dietary adjustments often involve reducing the intake of fats, salt, fiber, and gluten. While individual tolerance varies, there are common categories of foods widely recognized as potential aggravators for people with colitis. By limiting these, patients can better control their condition and avoid unpredictable flare-ups that interfere with daily life.
Gluten-rich foods such as wheat, rye, and barley are known to trigger symptoms in sensitive individuals, especially those with gluten sensitivities or celiac disease. These grains can cause inflammation and exacerbate gastrointestinal discomfort.
Alcoholic beverages are a major irritant to the gastrointestinal tract. Consuming alcohol can worsen inflammation, increase dehydration, and trigger flare-ups, especially when consumed on an empty stomach. Complete abstinence or significant reduction is often advised during active disease phases.
High-fiber foods such as legumes, including beans, peas, and lentils, along with fibrous vegetables like broccoli, cabbage, and Brussels sprouts, may induce bloating, cramping, and gas. To make these foods more digestible, cooking them thoroughly and removing skins and seeds is recommended. While fruits are generally healthy, those with seeds—like berries—or dried fruits may cause irritation and should be consumed cautiously. Fruit juices, particularly prune juice, are often better tolerated and can help maintain hydration.
Sulfates and sulfite-containing foods are compounds found naturally in red meats, dairy products, wine, beer, eggs, and certain cheeses. These substances can promote the growth of gut bacteria that produce toxic gases, leading to increased bloating, discomfort, and gas formation. Limiting intake of these foods can help alleviate these symptoms.
Nuts and Seeds—including sunflower, sesame, pumpkin seeds, and nuts like walnuts and cashews—are high in fiber and hard to digest, which can aggravate symptoms like bloating and abdominal pain. A low-fiber diet recommends minimizing or avoiding these ingredients during flare-ups.
Dairy products—such as milk, cheese, butter, and yogurt—may worsen symptoms, especially in individuals with lactose intolerance. Dairy can cause diarrhea, cramping, and increased gas in sensitive patients.
Caffeinated beverages like coffee, black and green teas contain caffeine, which can irritate the stomach lining, stimulate bowel movements, and induce diarrhea. Moderation or avoidance is advised during active inflammation stages.
Spicy foods—including chili peppers, hot sauces, and spicy seasonings—can cause significant irritation of the intestinal mucosa. Patients are often advised to limit or avoid these to prevent symptom aggravation.
Sugary foods and chocolate products—such as candies, sodas, chocolates, and sweet desserts—can worsen diarrhea and promote inflammatory responses due to their high sugar and caffeine content. Eliminating or reducing these can help better control symptoms and prevent flare-ups.
In addition to these dietary restrictions, maintaining a food diary and monitoring individual responses can help tailor a personal diet plan. Consulting with healthcare professionals or registered dietitians is essential for designing effective dietary strategies suitable for each patient’s specific condition and tolerance levels. Adopting a balanced, mindful approach to eating — emphasizing easily digestible, anti-inflammatory foods while avoiding known triggers — forms the cornerstone of managing ulcerative colitis successfully. Proper dietary management, alongside medication and lifestyle adjustments, can significantly improve disease control and enhance overall well-being for people living with colitis.