Comprehensive Guide to Recognizing and Managing Edema: Causes, Symptoms, and Treatments
This comprehensive guide explores edema, its signs, causes, and effective treatment options. It emphasizes the importance of early diagnosis and tailored management strategies for different underlying conditions like heart, liver, and kidney problems. Practical lifestyle tips and medical approaches help individuals manage swelling symptoms, improve circulation, and enhance overall health. Recognizing edema early and understanding its triggers can prevent complications and promote a better quality of life.

A Deep Dive into Edema: Recognizing Symptoms, Understanding Causes, and Exploring Effective Treatments
Edema, more commonly known as swelling, is a medical condition characterized by the accumulation of excess fluid in the body's tissues. This buildup results in visible puffiness, which can manifest in various parts of the body, most frequently in the lower extremities such as the legs and feet. However, edema can affect any part of the body, including the abdomen, face, and arms. Recognizing the signs early and understanding its underlying causes are crucial steps toward effective management and treatment.
Identifying the Symptoms of Edema
Swelling symptoms can vary depending on the affected area but typically include several recognizable signs. These include:
Shiny, stretched, or glossy skin over the swollen area
Skin that dents or pits when pressed inward (pit edema)
Feeling of heaviness or fullness, especially in the legs or ankles
In abdominal cases, bloating or a distended abdomen
In certain situations, redness or warmth—indicating possible infection or inflammation
Being aware of these signs helps in timely consultation with healthcare professionals to identify the root causes and prevent complications.
Common Causes and Underlying Health Conditions of Edema
Understanding the various factors that can lead to edema is vital. The condition often results from underlying health issues that affect fluid balance and circulation. Below are the primary causes:
1. Cardiac Problems
Heart failure, particularly when the heart's lower chambers are affected, impairs the heart’s ability to pump blood efficiently. This leads to blood backing up in the veins, causing fluid to seep into tissues, most notably in the legs, ankles, and abdomen. Pulmonary edema, a serious condition where fluid accumulates in the lungs, can also occur, resulting in breathing difficulties and coughing.
2. Liver Disorders
Liver conditions like cirrhosis cause increased pressure in the portal vein—the blood vessel supplying the liver—leading to fluid leakage into the abdominal cavity (ascites) and lower extremities. This causes distention and swelling, often accompanied by other symptoms like jaundice and weakness.
3. Kidney Dysfunction
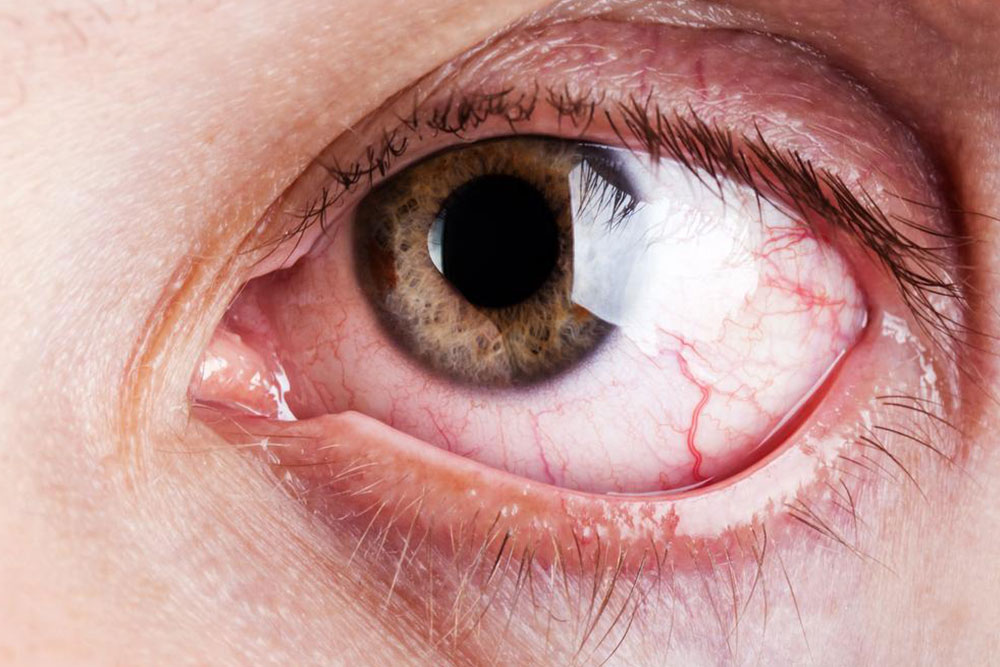
Kidneys play a pivotal role in maintaining fluid balance by filtering excess water and waste from the bloodstream. Kidney damage or disease, such as nephrotic syndrome, results in impaired filtration, leading to fluid retention and swelling, especially around the eyes, ankles, and legs.
4. Blood Clots and Circulatory Blockages
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, most commonly in the legs. This obstructs normal blood flow, causing localized swelling, pain, redness, and warmth. If untreated, it can lead to serious complications like pulmonary embolism.
Additional Factors Influencing Edema Development
Aside from primary medical conditions, certain lifestyle choices and environmental factors significantly contribute to edema:
Prolonged periods of immobility, such as sitting or standing for extended hours, hindering proper blood circulation
High intake of salt (sodium), which encourages water retention in the tissues
Weak immune systems, which can trigger infections or allergic reactions that cause swelling
Advancing age, which naturally decreases tissue elasticity and circulation efficiency
Cancer or tumors, which can alter blood substances and promote clot formation or fluid leakage
Strategies for Managing and Treating Edema Effectively
Prompt medical evaluation is essential for diagnosing the root causes of edema. Once identified, treatments are tailored to address specific underlying issues. Common management approaches include:
Implementing lifestyle modifications, such as increasing physical activity to improve circulation
Elevating the affected limbs above heart level to facilitate fluid drainage
Wearing compression stockings or sleeves to support venous return
Reducing salt intake to prevent excessive fluid retention
Taking prescribed medications, such as diuretics, to help eliminate excess fluid
Addressing the primary health conditions, like managing heart, liver, or kidney diseases through medication and therapy
In addition to medical treatments, adopting healthy habits can significantly improve symptoms. Regular exercise, maintaining a healthy weight, avoiding prolonged inactivity, and staying hydrated are crucial steps. Patients should seek regular follow-up care to monitor their condition and prevent recurrence.
Overall, understanding edema's causes and symptoms enables proactive management, minimization of risks, and enhancement of quality of life. Recognizing when to seek medical help and adhering to prescribed treatment plans can lead to effective control and improved health outcomes.