In-Depth Overview of Cervical Cancer Detection and Staging Procedures
This comprehensive guide covers cervical cancer diagnosis and staging, emphasizing the importance of early detection, screening methods, and advanced imaging techniques. With detailed information on symptoms, procedures, and disease stages, it aims to educate women and healthcare providers on effective management strategies. Early diagnosis through routine screenings greatly improves treatment success rates, highlighting the crucial role of regular check-ups and HPV vaccination. Understanding these processes fosters proactive health management and better survival outcomes for women worldwide.

In-Depth Overview of Cervical Cancer Detection and Staging Procedures
Cervical cancer remains a significant health concern for women worldwide, including in the United States. Annually, approximately 13,000 women receive a diagnosis of cervical cancer, making early detection and effective management crucial for improving survival rates. Despite the serious implications, advances in medical science have greatly contributed to a decline in mortality associated with cervical cancer. This progress is primarily attributable to enhanced screening techniques and widespread vaccination efforts against high-risk human papillomavirus (HPV), the primary cause of cervical cancer. Understanding the process of diagnosis and staging is vital for patients, caregivers, and healthcare professionals alike.
The origin of cervical cancer stems from abnormal cell growth within the cervix, which is the lower, narrow part of the uterus that connects to the vagina. Its development is closely linked to persistent infection with high-risk HPV types, a common sexually transmitted virus. While many HPV infections are cleared by the immune system without progressing further, a subset can remain dormant, leading to cellular abnormalities that may eventually evolve into malignant tumors. Several environmental and lifestyle factors, such as smoking, long-term oral contraceptive use, and a compromised immune system, can influence the risk of developing cervical cancer. The cornerstone of prevention includes HPV vaccination programs and regular screening tests, which can catch precancerous changes early, drastically reducing the progression to invasive cancer.
Diagnosing Cervical Cancer
Early diagnosis of cervical cancer hinges upon routine screening practices. The Pap smear, or Pap test, has been a standard method for detecting abnormal cervical cells since its introduction, and it is recommended for women starting at age 21. Alongside Pap smears, HPV DNA testing has gained prominence as a complementary screening technique, specifically identifying high-risk HPV infections that could lead to cancer.
When screenings reveal abnormal cells, further diagnostic procedures are necessary to establish a definitive diagnosis. The colposcope, a specialized magnifying instrument, allows clinicians to closely examine the cervical tissue and identify suspicious areas. For tissue confirmation, biopsy methods such as punch biopsy, endocervical curettage, or cone biopsy are performed. These procedures typically involve local anesthesia but can be done under general anesthesia depending on the case. The tissue samples obtained are examined microscopically by pathologists to determine the presence and nature of malignant cells, which confirms whether the lesion is cancerous.
Staging of Cervical Cancer
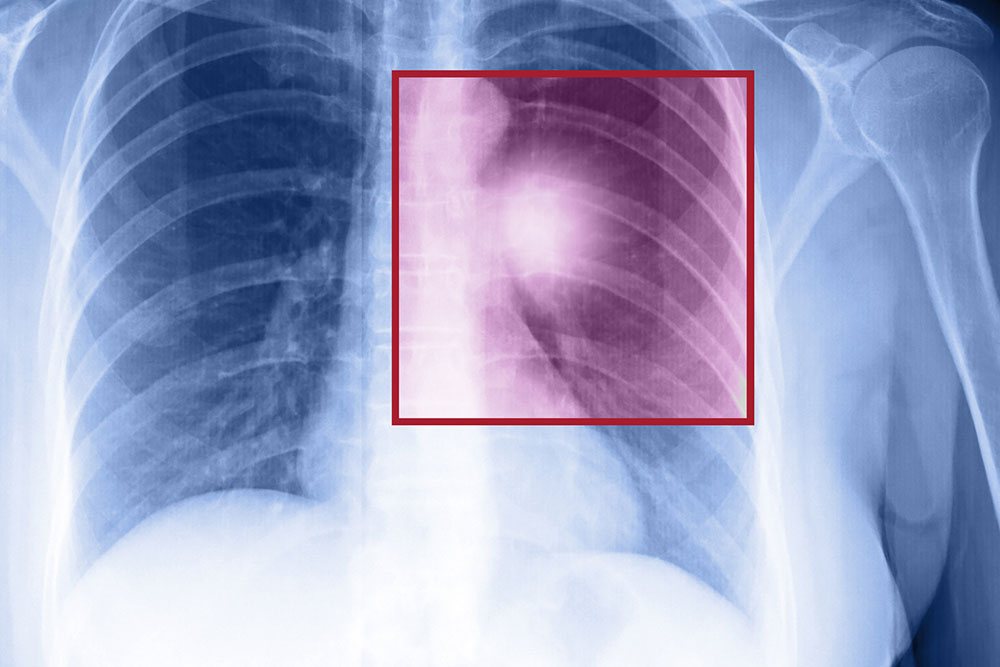
Once cervical cancer is diagnosed, determining the extent of the disease is critical for shaping an effective treatment plan. Staging involves a series of advanced imaging tests and examinations that assess whether the cancer has spread beyond the cervix into surrounding tissues or distant organs.
Imaging modalities such as Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET), Computed Tomography (CT), and standard X-rays play a vital role in this phase. These techniques provide detailed pictures that reveal the tumor size, local invasion, lymph node involvement, and distant metastasis. Additional scopes, such as rectal and bladder examinations, are sometimes used to evaluate invasion into nearby structures.
Based on these assessments, cervical cancer is classified into four stages, each indicating the severity and spread of the disease:
Stage 1: Cancer is confined within the cervix itself. When detected early at this stage, the prognosis is generally favorable, with high treatment success rates.
Stage 2: The malignancy extends beyond the cervix into the upper part of the vagina but has not reached the pelvic wall.
Stage 3: The cancer involves lower parts of the vagina, pelvic sidewalls, or causes kidney obstruction due to blockage of the ureters.
Stage 4: The most advanced stage, characterized by spread to nearby organs such as the bladder or rectum, or even distant sites like the bones or lungs.
Effective management of cervical cancer relies heavily on accurate staging. It guides clinicians in choosing appropriate treatment modalities, whether surgical removal, radiotherapy, chemotherapy, or targeted therapies. Early detection and precise staging significantly improve the outlook for women affected by this disease, emphasizing the importance of regular screening and prompt medical attention.
Overall, understanding the diagnostic and staging processes of cervical cancer empowers women and healthcare providers to make informed decisions, ultimately leading to better health outcomes and enhanced quality of life.