Comprehensive Guide to Lung Cancer: Symptoms, Diagnosis, and Risk Factors
This comprehensive article explores lung cancer’s symptoms, diagnostic methods, and risk factors, emphasizing the importance of early detection. It discusses the anatomy of the lungs, how mutations cause cancer, diagnostic procedures like biopsies and imaging, and risk factors such as smoking, environmental exposure, and genetics. Recognizing early signs and understanding risk factors play a pivotal role in improving survival rates. The article highlights preventive strategies, advances in diagnosis, and the significance of public health efforts to combat lung cancer worldwide.

Comprehensive Guide to Lung Cancer: Symptoms, Diagnosis, and Risk Factors
Lung cancer remains one of the most prevalent and deadly types of cancer worldwide. Understanding its complexities, including symptoms, diagnostic procedures, and risk factors, is crucial for early detection and effective treatment. The lungs are vital organs responsible for gas exchange—absorbing oxygen and expelling carbon dioxide—serving as the cornerstone of respiratory health.
The structure of the lungs comprises various cell types, predominantly epithelial cells lining the airways, along with blood vessels, nerves, structural tissues, and hormone-producing cells. These epithelial cells produce mucus, which acts as a protective barrier, trapping dust, microbes, and other particles to prevent damage to lung tissues. Lung cancer arises when genetic mutations disrupt normal cell growth and division processes, leading to uncontrolled proliferation. Mutated epithelial cells can form tumors that either remain localized or invade neighboring tissues, and in advanced stages, metastasize to other parts of the body.
Diagnosing lung cancer promptly is essential for improving prognosis and treatment outcomes. The diagnostic process involves a combination of clinical evaluations, imaging studies, laboratory tests, and histopathological examinations.
Biopsy: A definitive diagnosis of lung cancer relies on obtaining tissue samples through biopsy procedures, examined under microscopes to identify malignant cells. Techniques include transthoracic needle biopsy, bronchoscopy, and surgical biopsies, each chosen based on tumor location and patient condition.
Medical History: A thorough review of the patient’s medical history helps identify risk factors and potential causes. This includes assessing prior respiratory illnesses, family history of cancer, occupational exposures, smoking history, and environmental factors.
Laboratory Tests: Blood tests evaluate overall health, organ function, and detect paraneoplastic syndromes associated with lung tumors. Sputum cytology examines mucus expectorated from the lungs to detect abnormal cells, aiding in diagnosis, though less sensitive than imaging.
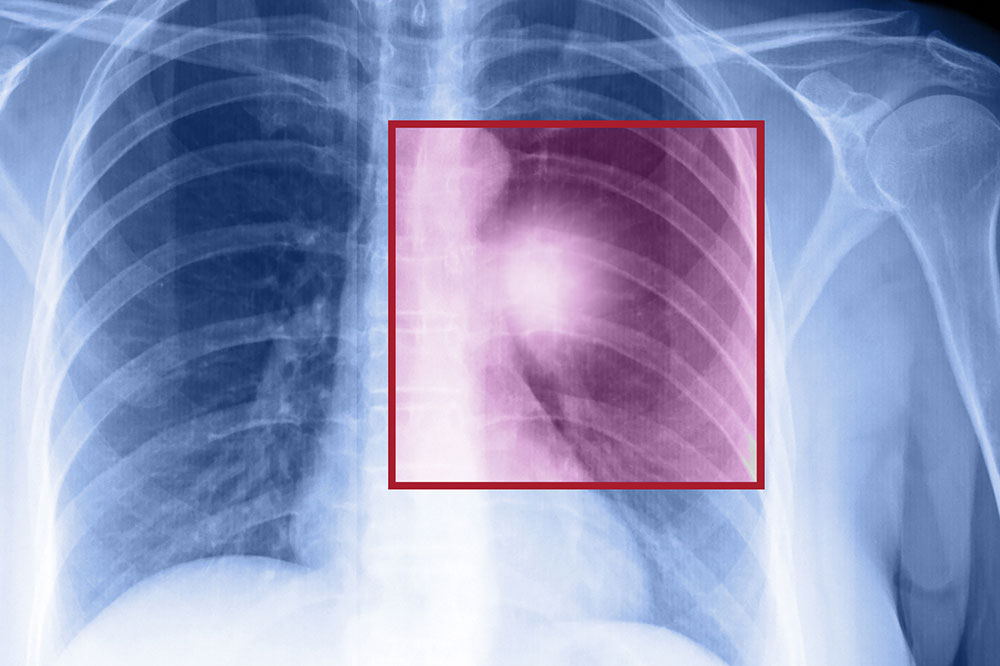
Imaging Studies: Advanced imaging techniques are vital for locating tumors, determining their size, and assessing the extent of disease spread. Chest X-rays are often initial tests, but CT scans provide detailed cross-sectional images. PET scans help identify active cancerous tissues and metastasis, whereas MRI and Bone scans further evaluate neurological or skeletal involvement.
Many lung cancers are asymptomatic in early stages, making regular screening essential, especially for high-risk groups. As the disease progresses, symptoms become more noticeable and concerning. Common early signs include a persistent cough that doesn’t resolve, blood in sputum (hemoptysis), chest pain, hoarseness, breathlessness, fatigue, recurrent respiratory infections, and wheezing. These symptoms often mimic benign respiratory conditions, contributing to delayed diagnosis.
In advanced cases, where metastasis has occurred, symptoms can broaden to include back pain, persistent headaches, weakness or numbness, jaundice, and neurological deficits depending on affected organs. Recognizing these signs promptly can facilitate early intervention, potentially improving survival rates.
Several factors increase the risk of developing lung cancer. Cigarette smoking remains by far the most significant risk factor, accounting for approximately 85% of cases. The risk increases with the duration and intensity of smoking, but even passive exposure to tobacco smoke elevates risk. Occupational exposures to carcinogens such as asbestos, arsenic, diesel exhaust, and certain metals like chromium and nickel greatly contribute to lung cancer development among workers in specific industries.
Environmental pollutants are also associated with increased risk. Air pollution, especially fine particulate matter (PM2.5), has been linked to lung cancer incidence. Additionally, individuals with a family history of lung cancer may carry genetic predispositions, although this account is less common compared to environmental and lifestyle factors. Prior lung illnesses, like chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis, can also predispose individuals to lung cancer. Moreover, exposure to radiation—whether from medical treatments or environmental sources—can increase risk, particularly if exposure is prolonged or intense.
Understanding these risk factors and recognizing early symptoms can significantly impact prognosis. Strategies such as smoking cessation programs, workplace safety regulations, air quality improvements, and routine screening for high-risk populations are important measures for prevention and early detection.
In summary, lung cancer is a complex disease requiring a multifaceted approach for diagnosis and management. Awareness about risk factors, early signs, and diagnostic procedures can lead to earlier detection, thereby improving treatment options and survival chances. Advances in imaging, targeted therapy, and minimally invasive biopsies continue to enhance patient outcomes. Public health campaigns aimed at reducing smoking and occupational hazards are essential in decreasing the global burden of lung cancer.