Comprehensive Guide to Ulcerative Colitis: Causes, Symptoms, Diagnosis, and Modern Management Techniques
This comprehensive guide explores ulcerative colitis, including its causes, symptoms, diagnostic methods, and the latest management strategies. It aims to increase awareness and understanding of this chronic inflammatory bowel disease, highlighting the importance of early diagnosis and personalized treatment options to improve patient outcomes and quality of life.

Comprehensive Guide to Ulcerative Colitis: Causes, Symptoms, Diagnosis, and Modern Management Techniques
Ulcerative colitis (UC), alongside Crohn’s disease, is one of the most prevalent inflammatory bowel diseases (IBD) affecting millions of individuals globally. This chronic condition is characterized by inflammation and ulcer formation within the lining of the large intestine, primarily affecting the rectum and colon. It can significantly impact quality of life, leading to persistent discomfort, anemia, and other health complications. In the United States alone, approximately 1.3% of adults, which translates to millions of individuals, are diagnosed with UC. Understanding this disease, its causes, symptoms, diagnostic processes, and emerging management strategies is crucial in improving patient outcomes and quality of life.
Understanding the underlying causes of ulcerative colitis
Despite extensive research, the exact etiology of ulcerative colitis remains elusive. However, scientists have identified several factors that likely contribute to its development. These include genetic predispositions, environmental influences, and immune system irregularities. These elements may act independently or synergistically, triggering the onset of UC. Let’s delve into these contributing factors in greater detail to understand their roles better.
Genetic factors in ulcerative colitis
Evidence from familial and twin studies suggests that genetics play a significant role in UC susceptibility. Certain genetic markers have been identified in individuals with a family history of the disease, indicating inherited predispositions. For example, variations in genes related to immune regulation and epithelial barrier function have been linked to increased risk. Nevertheless, these genetic factors alone do not guarantee disease development, implying a complex interaction with environmental factors. Ongoing research continues to uncover new genetic loci associated with UC, aiming to provide insights into personalized treatment options in the future.
Environmental triggers influencing ulcerative colitis
Environmental factors are believed to substantially influence the onset and flare-ups of UC. These include dietary habits, medication usage, and exposure to certain environmental agents. Studies have shown that medications such as non-steroidal anti-inflammatory drugs (NSAIDs), oral contraceptives, and antibiotics can increase UC risk or exacerbate existing symptoms. Diets high in processed foods, unhealthy fats, and sugar may also contribute to inflammation and gut dysbiosis, aggravating disease activity. Additionally, chronic stress and lifestyle factors like smoking or not engaging in regular physical activity have been associated with increased susceptibility and severity of ulcerative colitis. Understanding these influences empowers patients and healthcare providers to adopt preventative strategies and modify risk factors through lifestyle adjustments.
Immune response abnormalities in ulcerative colitis
A hallmark of ulcerative colitis is an abnormal immune response. Under normal circumstances, the immune system protects the body against pathogens without harming healthy tissues. In UC, this regulation fails, leading to an overactive immune response targeting the cells lining the colon. This misguided attack results in inflammation, ulcer formation, and tissue damage. The immune dysregulation involves complex interactions between various immune cells, cytokines, and signaling pathways. Emerging therapies aim to modulate these immune responses, providing targeted treatments to reduce inflammation and promote mucosal healing.
Recognizing the symptoms of ulcerative colitis
The clinical presentation of ulcerative colitis varies from mild to severe. Common symptoms include abdominal pain and cramping, often localized to the lower left quadrant, along with frequent diarrhea, which may contain blood and mucus. Patients often experience urgency to defecate and feelings of incomplete evacuation. Other notable symptoms include rectal bleeding, fatigue, weight loss, fever, and anemia due to chronic blood loss. In some cases, extra-intestinal manifestations occur, such as joint pain, eye irritation, skin rashes, and sore mouth, reflecting systemic immune activation.
Initially, symptoms tend to be mild and intermittent, but if untreated, they can worsen over time, leading to severe complications like toxic megacolon or increased risk of colon cancer. Recognizing these symptoms early and seeking prompt medical attention is vital for effective management and improved prognosis.
Diagnosing ulcerative colitis: Methods and challenges
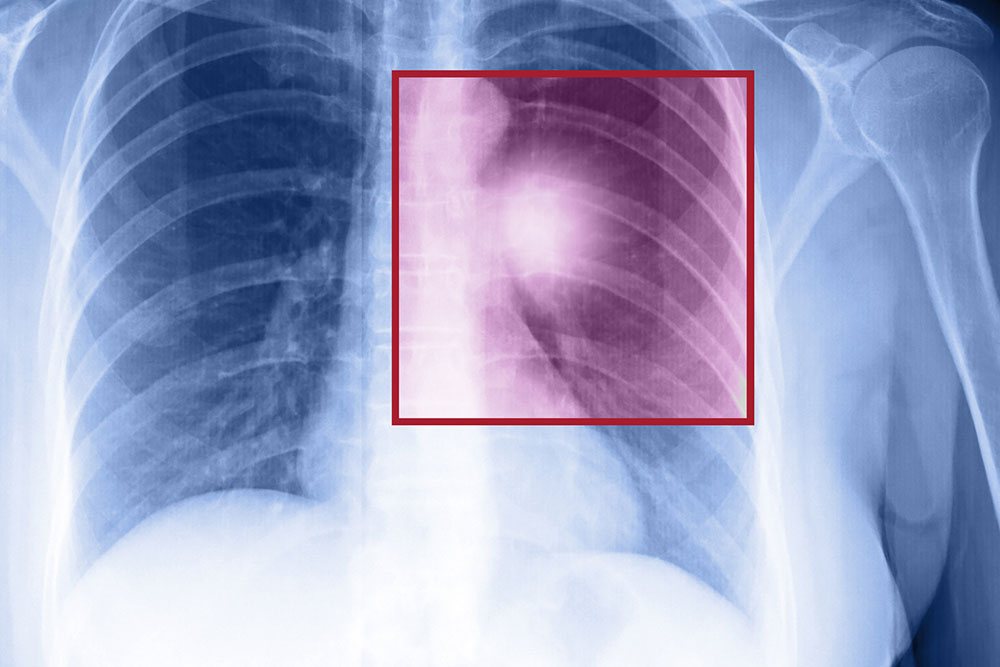
Accurate diagnosis of ulcerative colitis involves a combination of clinical evaluation, laboratory investigations, and endoscopic procedures. Physical examination focuses on checking for abdominal tenderness, signs of anemia, and other systemic signs of inflammation. Blood tests, including complete blood count (CBC), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR), help assess inflammation severity. Stool tests rule out infections and other causes of diarrhea.
An essential diagnostic tool is endoscopy, particularly colonoscopy, which allows direct visualization of the colonic mucosa. During the procedure, biopsies are obtained to confirm inflammation, distinguish UC from Crohn’s disease, and assess for dysplasia or early cancer. Sigmoidoscopy may be used for initial assessments. Additional imaging techniques like barium enemas or intestinal ultrasound may sometimes be employed.
Differentiating UC from other gastrointestinal disorders such as irritable bowel syndrome (IBS), celiac disease, and infectious colitis is crucial for effective treatment planning. While diagnosis can sometimes be challenging due to overlapping symptoms, comprehensive evaluation improves accuracy and helps tailor treatment approaches.
Modern treatment approaches for ulcerative colitis
The management of ulcerative colitis has advanced considerably, aiming to induce and maintain remission, reduce symptoms, and prevent complications. Treatment strategies are personalized based on disease severity, extent, patient response, and comorbidities. Medications are the cornerstone of therapy, with options including aminosalicylates, corticosteroids, immunomodulators, and biologic agents.
Aminosalicylates, such as mesalamine, help reduce inflammation in the colon lining and are often employed for mild to moderate disease. Corticosteroids are effective during flare-ups but are used short-term due to adverse side effects. Immunomodulators like azathioprine and methotrexate suppress immune activity and are useful for maintaining remission.
Biologics—monoclonal antibodies targeting specific immune proteins such as TNF-alpha inhibitors—have revolutionized UC treatment, especially for moderate to severe cases that don’t respond to conventional therapies. These drugs significantly reduce inflammation and promote mucosal healing, improving patients’ quality of life.
In some severe cases or when medical management fails, surgical interventions such as colectomy (removal of the colon) may be necessary. Surgery can be curative but involves lifestyle adjustments and potential impacts on bowel function. Ongoing research is focused on developing targeted therapies with fewer side effects and improved safety profiles.
In addition to medications, lifestyle modifications — including a balanced diet, stress management, smoking cessation, and regular exercise — can support disease control. Monitoring for complications, such as colon cancer, with routine colonoscopies is also a vital aspect of long-term management.
Overall, the goal is to achieve remission, improve the patient’s quality of life, and prevent disease-related complications through a combination of personalized medical treatment, lifestyle adjustments, and regular monitoring.