Comprehensive Lifestyle Strategies for Managing Ankylosing Spondylitis Effectively
Discover 8 comprehensive lifestyle strategies to effectively manage ankylosing spondylitis. From nutrition and exercise to ergonomic work setups and mental health, this detailed guide offers practical tips for improving quality of life and controlling symptoms of this chronic condition. Embrace these lifestyle changes to maintain mobility, reduce pain, and enhance overall well-being.

8 Proven Lifestyle Approaches to Managing Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a long-term inflammatory disease primarily affecting the spine and sacroiliac joints, which link the base of the spine to the pelvis. This condition often leads to severe pain, stiffness, and progressive fusion of the vertebrae, causing a reduction in spinal flexibility and the development of a hunched or stooped posture. The inflammation can sometimes extend beyond the spine, impacting other joints and organs such as the eyes and lungs, resulting in a broader spectrum of health issues. Although there is currently no cure for ankylosing spondylitis, adopting certain lifestyle modifications can dramatically enhance a patient's quality of life and help manage symptoms effectively. This comprehensive guide explores key strategies to cope with the condition, emphasizing sustainable habits and proactive approaches.
Optimized Nutrition and Dietary Choices: While no specific diet cures AS, nutrition plays a vital role in managing inflammation and supporting overall health. Incorporating anti-inflammatory foods such as fatty fish rich in omega-3 fatty acids (like salmon, mackerel, and sardines) can help reduce joint inflammation. Whole grains, fresh fruits, and vegetables contribute essential nutrients and antioxidants that combat oxidative stress. Additionally, herbs like turmeric and ginger have natural anti-inflammatory properties and can be included in meals. Calcium-rich foods such as dairy products or leafy greens maintain bone strength, crucial given the risk of osteoporosis and bone fusion. Maintaining a healthy weight reduces undue pressure on weight-bearing joints, alleviating discomfort. An anti-inflammatory diet not only helps control pain but also enhances energy levels and overall mobility.
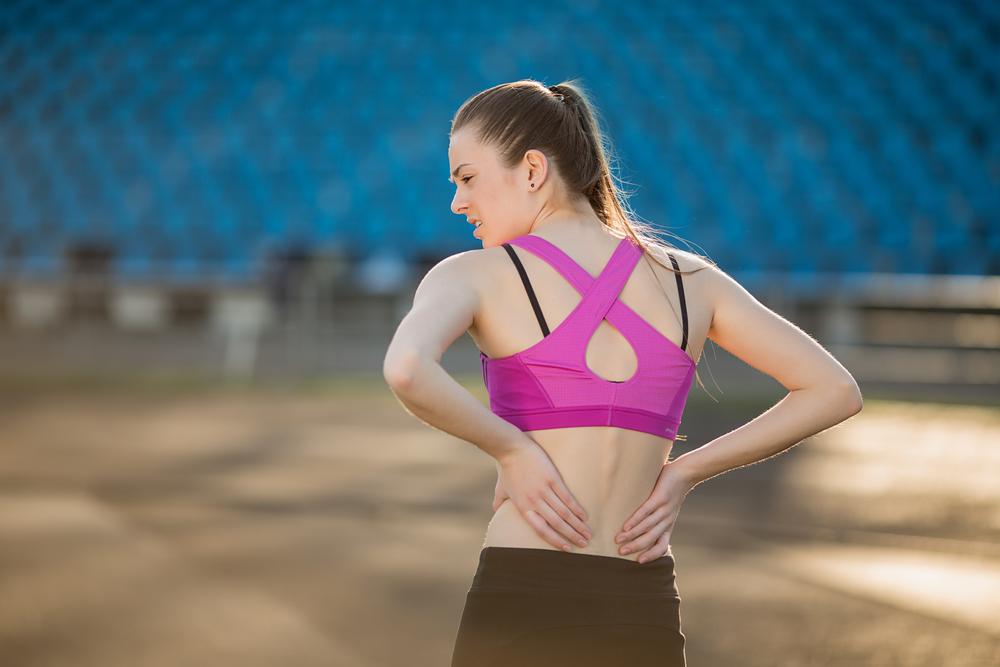
Engaging in Consistent, Gentle Exercise: Regular physical activity is essential for maintaining joint mobility, muscle strength, and cardiovascular health. Low-impact exercises such as swimming, water aerobics, cycling, and brisk walking are highly recommended, as they exert less stress on the joints compared to high-impact activities. These activities help preserve flexibility, improve posture, and aid weight management. It’s important to listen to your body's signals; if an activity increases discomfort or pain, modify the routine accordingly or stop to prevent injury. Working with a healthcare professional or physical therapist can optimize the exercise plan, ensuring it is safe and tailored to your specific needs. Staying active also releases endorphins, which are natural pain relievers and mood lifters—crucial for managing the emotional burden of chronic illness.
Seeking Specialized Physical Therapy: Professional physical therapy plays a vital role in managing ankylosing spondylitis. A qualified therapist develops personalized stretching and strengthening routines to improve posture, reduce stiffness, and enhance range of motion. Techniques may include joint mobilization, myofascial release, and targeted exercises to strengthen core muscles. Applying heat can help relax tense muscles, while cold packs can relieve inflammation and pain during flare-ups. Regular therapy sessions combined with at-home exercises significantly contribute to long-term mobility and symptom control. Education on posture, breathing techniques, and ergonomic practices forms a core part of therapy, empowering patients to manage daily activities more effectively.
Creating a Supportive and Ergonomic Work Environment: For many individuals, work-related activities can exacerbate symptoms if not properly managed. Jobs involving heavy lifting, repetitive movements, or prolonged periods of sitting may aggravate joint pain and stiffness. Adapting the workspace ergonomically is crucial; this includes supportive chairs, adjustable desks, and appropriate equipment that minimizes strain. Incorporating frequent stretching breaks during work hours helps prevent stiffness and muscle tightness. If possible, opt for flexible work arrangements or modify workload to reduce physical stress. Consulting with occupational therapists can provide valuable insights into ergonomic modifications that suit individual needs, enabling better disease management during working hours.
Prioritizing Rest and Quality Sleep: Adequate sleep is a cornerstone of managing chronic pain and fatigue associated with ankylosing spondylitis. Developing a consistent sleep routine helps regulate the body's internal clock. It's advisable to avoid caffeine and heavy meals close to bedtime, and to establish a calming pre-sleep ritual. Using a supportive pillow can maintain proper spinal alignment during rest, reducing morning stiffness. If discomfort interferes with sleep, techniques such as warm baths or gentle stretches before bed can be beneficial. Sleep disturbances can exacerbate pain perception and overall fatigue, so addressing sleep hygiene is vital for maintaining daily functioning and emotional resilience.
Maintaining Proper Posture and Body Mechanics: Correct posture is essential to prevent further spinal curvature and joint stress. Regularly practicing posture awareness and incorporating core stabilization exercises strengthen the muscles that support the spine. Avoid slouching and maintain ergonomic alignment during daily activities, especially when sitting at a desk or using a mobile device. Using back support cushions and standing desks can help maintain spinal health. Continuous attention to correct postures reduces strain and minimizes the progression of spinal deformities, ultimately alleviating pain and improving mobility over time.
Effective Pain Management Techniques: Managing pain during flare-ups requires a combination of approaches. Cold packs and ice therapy can effectively reduce inflammation and numbness. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed under medical supervision. Complementary therapies such as acupuncture, massage, and mindfulness-based stress reduction can provide additional relief. Developing an individualized pain management plan in collaboration with healthcare professionals ensures that pain is controlled without reliance solely on medications, reducing potential side effects. Employing relaxation techniques and staying mentally positive can also influence the perception of pain, contributing to overall well-being.
Building a Resilient Mental and Emotional Outlook: Living with a chronic condition like ankylosing spondylitis is emotionally taxing. Cultivating a positive attitude, seeking support from friends, family, or support groups, and practicing stress management techniques are essential for mental health. Setting realistic goals and celebrating small victories foster a sense of achievement and control. Engaging in hobbies, mindfulness meditation, and counseling can help cope with emotional challenges. Supporting mental health not only improves quality of life but also has a favorable impact on physical symptoms, creating a holistic approach to managing ankylosing spondylitis.