Comprehensive Approaches to Managing Irritable Bowel Syndrome Effectively
This comprehensive guide explores effective strategies for managing Irritable Bowel Syndrome (IBS). Covering diagnosis, lifestyle changes, dietary management, and medication options, it offers personalized approaches for symptom relief. Regular monitoring, avoiding triggers, and collaborating with healthcare providers can significantly improve quality of life for IBS sufferers. The article emphasizes the importance of tailored treatments and lifestyle adjustments, providing valuable insights for those seeking effective IBS management methods.

Comprehensive Approaches to Managing Irritable Bowel Syndrome Effectively
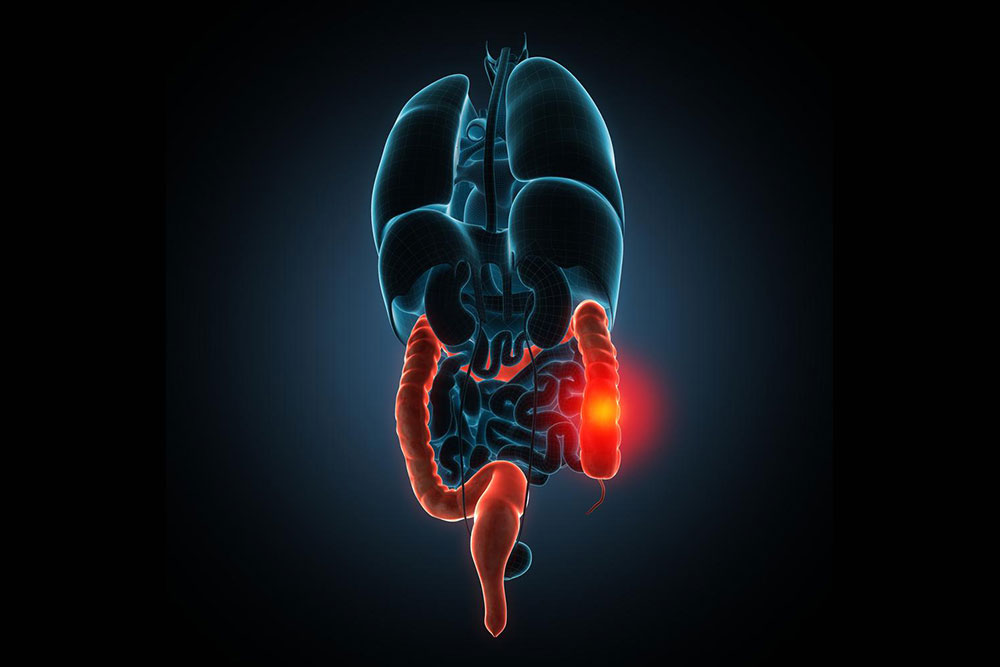
Irritable Bowel Syndrome (IBS) remains one of the most prevalent gastrointestinal disorders worldwide, affecting millions of individuals with persistent symptoms such as abdominal pain, bloating, cramping, and irregular bowel habits. These symptoms may manifest as constipation, diarrhea, or alternating patterns, significantly impacting patients' quality of life. Despite its chronic nature, IBS does not typically lead to more severe conditions like inflammatory bowel disease or colorectal cancer. Its diagnosis often involves a systematic process of elimination, including various laboratory tests, because the precise etiology remains elusive.
This condition has multifactorial origins. Contributing factors include heightened nerve sensitivity within the gut, abnormal muscle contractions of the gastrointestinal tract, ongoing mucosal inflammation, and psychological aspects such as stress or anxiety. The complex interplay of these factors makes personalized treatment plans crucial for effective management.
Personalized treatment strategies depend largely on the severity of symptoms, their specific characteristics, and the degree to which they interfere with daily functioning. As no single medication effectively addresses all symptoms for every patient, collaborative efforts with healthcare providers—including gastroenterologists, dietitians, and mental health professionals—are essential. Lifestyle modifications, dietary adjustments, and behavioral therapies often form the cornerstone of symptom control and overall management.
Identify your primary symptoms and assess their impact on daily life
Monitor symptoms over several weeks to detect patterns and potential triggers
Avoid known dietary triggers such as spicy foods, caffeine, and processed snacks
Implementing specific lifestyle and dietary changes can substantially ease symptoms of IBS. Below are detailed recommendations to help manage and alleviate discomfort:
Limit intake of caffeine, alcohol, and fatty foods which can irritate the gut
Reduce consumption of dairy products, certain fruits like apples and pears, and artificial sweeteners if diarrhea is predominant
Increase dietary fiber intake primarily through fruits, vegetables, and legumes to promote bowel regularity and reduce bloating
Avoid gas-producing foods such as beans, raw cabbage, broccoli, and cauliflower to minimize gas and bloating
Engage in regular physical activity, such as walking, cycling, or swimming, to enhance digestion, boost energy levels, improve sleep quality, and promote emotional well-being
Cease smoking to improve overall gastrointestinal health and reduce symptom severity
Use prescribed medications appropriately for diarrhea, constipation, or abdominal cramps, as directed by your healthcare provider
Implement stress management techniques such as mindfulness, meditation, or counseling to alleviate psychological triggers
Diagnostic Procedures for IBS
Diagnosing IBS primarily involves a comprehensive assessment of symptoms and careful exclusion of other medical conditions. Common diagnostic procedures include:
Detailed review of medical history
Thorough physical examination
Blood tests to exclude celiac disease and other systemic issues
Complete blood count (CBC) to check for anemia or infection
Inflammation markers, such as sedimentation rate or C-reactive protein (CRP)
Stool analysis to detect infections, blood, or malabsorption
Additional investigations like thyroid function tests or colonoscopy if warranted
Targeted Medications for Managing IBS
Medications are tailored to specific symptoms and may include:
Antidiarrheal agents such as loperamide and diphenoxylate to control diarrhea
Bile acid sequestrants like cholestyramine to reduce diarrhea symptoms
Rifaximin (Xifaxan), an antibiotic that can reduce bacterial overgrowth contributing to bloating and diarrhea, typically used for a 14-day course
Alosetron, a receptor antagonist prescribed for severe diarrhea predominant IBS, but used under strict medical supervision due to potential adverse effects
Relief Options for Constipation
For patients primarily experiencing constipation, over-the-counter remedies are often effective, but consultation with a healthcare professional is recommended before initiation. Common options include:
Osmotic laxatives such as Milk of Magnesia and lactulose which draw water into the intestines
Polyethylene glycol-based products like MiraLax that improve stool consistency
Stimulant laxatives like Senokot, used occasionally and with caution
Medications specifically approved for IBS-related constipation, including Linaclotide (Linzess) and Lubiprostone (Amitiza)
If symptoms persist despite primary treatments, consulting a gastroenterologist or mental health professional can provide further management options, especially if psychological factors like stress exacerbate symptoms.