Comprehensive Guide to Managing Opioid Dependence: Withdrawal Symptoms and Effective Recovery Strategies
This comprehensive guide explores the symptoms of opioid withdrawal, effective treatment options, and strategies for recovery. Medical support, medication management, and behavioral therapies are emphasized as key components for overcoming dependence. Understanding these aspects can empower patients and caregivers to navigate detoxification safely and achieve sustained recovery from opioid addiction.

In-Depth Understanding of Opioid Withdrawal and Effective Treatment Options
Recognizing the Symptoms of Opioid Withdrawal:
Opioid dependence presents with a complex set of withdrawal symptoms that occur in distinct phases. Understanding these symptoms is critical for effective treatment and recovery. The initial phase of withdrawal usually manifests within hours to a few days after cessation or reduction of opioid use. Common early symptoms include a combination of physical and psychological effects such as severe fatigue, persistent yawning, difficulty sleeping (insomnia), excessive sweating, a runny nose, watery eyes, heightened agitation, anxiety, restlessness, and muscle discomfort. These early signs can make the process of detoxification uncomfortable but are typically manageable with proper medical oversight.
As withdrawal progresses, individuals often experience more intense physical reactions, marking the second stage. This phase can include symptoms such as the development of goosebumps (sometimes referred to as 'cold flashes'), a rapid heartbeat, dilated pupils, nausea with possible vomiting, stomach cramps, and diarrhea. These symptoms can persist from a few days up to several weeks, depending on the severity of dependence and individual health factors. Besides the immediate physical discomfort, long-term withdrawal can induce significant behavioral and emotional challenges, including mood swings, depression, anxiety, and difficulty concentrating, which require targeted therapeutic interventions.
Complete detoxification from opioids is rarely achievable without medical support due to the severity and duration of withdrawal symptoms. Healthcare professionals often prescribe medications that help mitigate cravings, ease withdrawal discomfort, and prevent relapse. These medications are tailored to each patient's needs and are usually administered under careful supervision, often involving gradual dose tapering over a period extending beyond six months. The goal of medically supervised detox is to stabilize the patient physically and psychologically, facilitating long-term recovery.
Pharmacological treatment is a cornerstone in managing opioid dependence. These medications reduce the risk of relapse by controlling cravings and alleviating withdrawal symptoms. Physicians typically implement a gradual tapering approach, carefully adjusting medication dosages over time to support the patient's withdrawal process and promote sustained recovery. Several medications are commonly used in this treatment protocol:
Buprenorphine: A partial opioid agonist that binds to brain receptors involved in pain and reward, tricking the brain into perceiving sufficient opioid activity without producing the euphoric high. It effectively reduces withdrawal symptoms and cravings while lowering overdose risks.
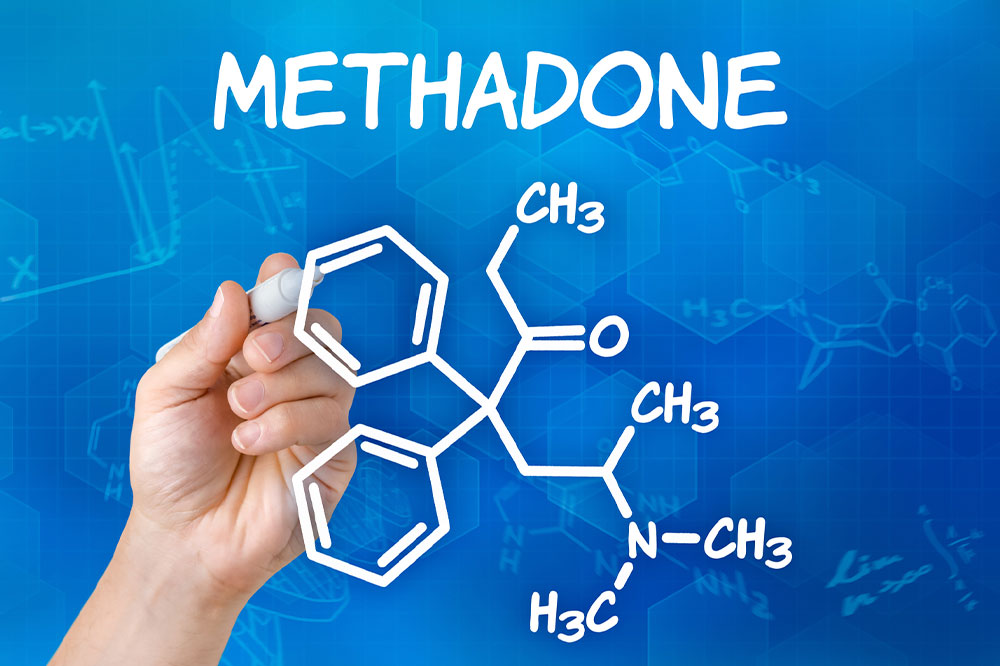
Methadone: A long-acting opioid agonist that alleviates withdrawal discomfort, diminishes cravings, and blocks the euphoric effects of other opioids, typically providing relief for about 24 hours. It is administered in specialized clinics to ensure proper dosing and safety.
LAAM (Levo-alpha-acetyl-methadol): An alternative to methadone, LAAM extends the duration of action, reducing cravings and withdrawal signs for over 72 hours. It works by dampening the euphoric effects, making it easier for patients to abstain from illicit opioid use.
Naltrexone: An opioid antagonist used after detoxification to prevent relapse. It blocks opioid receptors, eliminating the effects of both prescribed and illicit opioids, thereby discouraging their use and aiding long-term abstinence.
Additional Support Medications: Various drugs like Trazodone (for sleep), Buprenorphine Subutex, Methocarbamol (muscle relaxant), Dicyclomine hydrochloride (stomach cramping relief), Clonidine (for withdrawal symptoms like sweating and agitation), along with antiemetics and antidiarrheals, are used as supportive measures to manage specific symptoms and hasten recovery.
Beyond medication, psychological support, counseling, and behavioral therapies play a vital role in managing addiction. The combined approach of pharmacotherapy and counseling increases the chances of long-term recovery by addressing underlying behavioral issues, improving emotional stability, and reducing the risk of relapse. Overall, comprehensive management involving both medical and psychological components is essential for overcoming opioid dependence and returning to a healthy, productive life.