Comprehensive Guide to How Diabetes Affects Foot Health and Preventive Strategies
This comprehensive guide explains how diabetes affects foot health, highlighting the underlying causes like poor circulation and nerve damage. It details common foot issues such as infections, deformities, and skin problems, emphasizing preventive care and management strategies. By understanding these connections, diabetics can take proactive measures to avoid serious complications, including ulcers and amputations, ensuring better foot health and overall quality of life.

Diabetes mellitus, commonly known as diabetes, is a complex chronic health condition characterized by the body's inability to produce enough insulin or effectively use the insulin it produces. Insulin, a hormone produced by the pancreas, plays a crucial role in converting the food we eat into energy. When the body fails to regulate blood sugar levels properly, it results in elevated blood glucose, which over time can lead to a wide range of health complications affecting various organs and tissues.
High blood sugar levels, if unmanaged, can cause damage to blood vessels, nerves, and tissues throughout the body. This damage is responsible for many of the serious health issues associated with diabetes, including cardiovascular disease, eye problems such as retinopathy, kidney failure, and importantly, nerve damage, particularly in the extremities. Among these complications, diabetic foot problems are especially significant because they can severely impair mobility and quality of life, and may even result in limb amputations if not properly managed.
Understanding the connection between diabetes and foot health is vital for preventing complications. The primary pathways through which diabetes harms foot health involve decreased blood circulation and peripheral neuropathy. These conditions create a dangerous environment where minor injuries can escalate into serious infections or gangrene, often requiring surgical intervention.
This comprehensive guide aims to explain the mechanisms by which diabetes impacts the feet, outline common foot complications associated with diabetic patients, and highlight effective prevention and management strategies to minimize risks.
The Pathophysiology of Diabetic Foot Problems
The development of foot problems in diabetics stems largely from two main issues: impaired blood flow and nerve damage. Elevated blood glucose levels damage blood vessels, leading to narrowing or occlusion of small arteries that supply the feet. This reduced circulation limits the delivery of oxygen and nutrients essential for tissue repair, making the skin and underlying tissues vulnerable to injury and slow to heal.
Simultaneously, uncontrolled blood sugar damages peripheral nerves, resulting in diabetic peripheral neuropathy. Nerve impairment causes numbness, tingling, or burning sensations in the feet and legs, which may decrease the patient’s ability to detect injuries, cuts, blisters, or pressure points. Consequently, injuries may go unnoticed and untreated, increasing the risk of infections that can become severe or even life-threatening if not addressed timely.
Common Foot Complications in Diabetes
Diabetes influences foot health through a variety of specific issues, many of which are interconnected. Awareness of these problems is essential for timely intervention and prevention.
Fungal Infections: Fungal infections such as athlete's foot and nail fungus are common among diabetics. They lead to discoloration, inflammation, and pain in the toenails and skin. If untreated, these infections can penetrate deeper tissues, causing more widespread infections and impairing mobility.
Musculoskeletal Problems: Nerve damage and poor circulation can result in musculoskeletal issues such as deformities, tendon issues, and balance problems. These conditions increase the risk of falls and injuries, which can be catastrophic if not managed properly.
Calluses and Corns: Repeated pressure and friction from ill-fitting footwear cause thickened skin patches, known as calluses and corns. These can distort foot alignment and increase the risk of ulcers.
Bunions: Bony deformities characterized by lateral deviation of the big toe often develop due to muscle imbalance, footwear pressure, and joint degeneration. Severe bunions can interfere with walking and may require surgical correction.
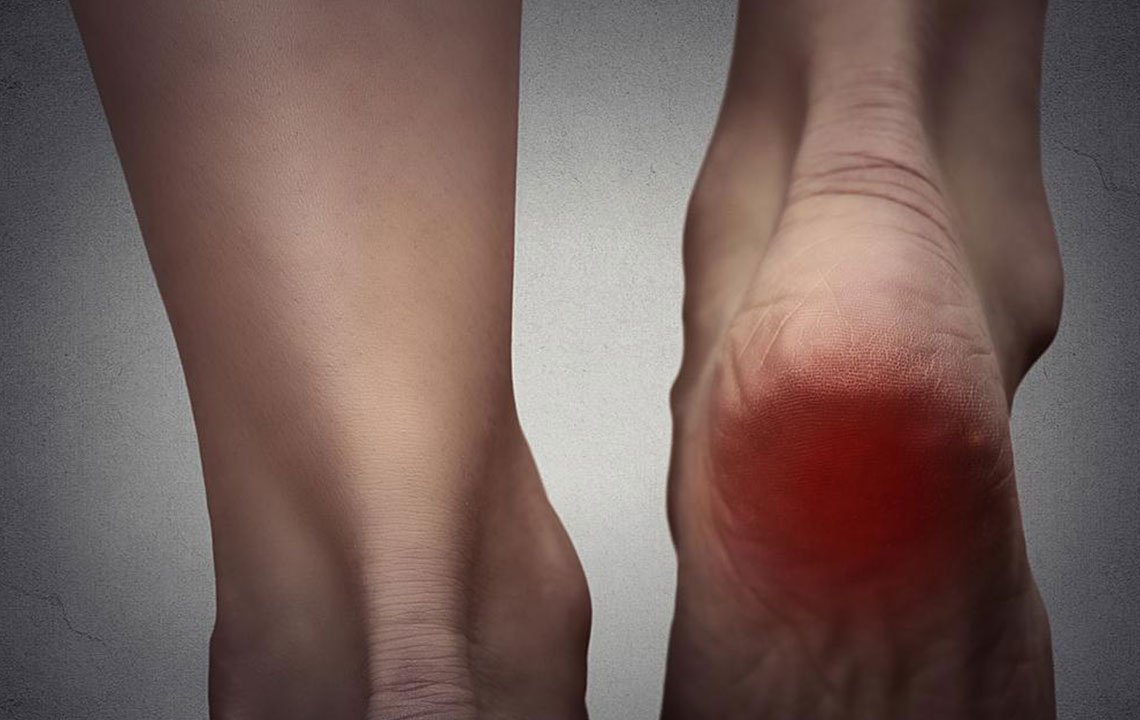
Dry, Cracked Skin: The skin on diabetic feet often becomes dry and cracked, especially around the heels. Cracks can serve as entry points for bacteria, leading to infections that are difficult to heal in diabetic individuals.
Preventive Measures and Care Strategies
Prevention is the cornerstone of managing diabetic foot health. Regular foot care routines, early detection of problems, and lifestyle adjustments significantly reduce the risk of complications.
Daily Foot Inspection and Hygiene
Patients should inspect their feet daily for any cuts, blisters, redness, swelling, or signs of infection. Maintaining good foot hygiene by washing with lukewarm water and gentle soap, followed by thorough drying—especially between the toes—is essential. Moisturizing the skin helps prevent cracks but should be avoided between the toes to prevent fungal growth.
Proper Footwear
Wearing well-fitting shoes that provide adequate support and cushioning can prevent pressure points, calluses, and other injuries. Custom orthotics may be recommended for individuals with deformities or high-pressure areas. Avoiding tight or high-heeled shoes is advised to maintain proper foot alignment and circulation.
Regular Medical Check-Ups
Annual foot examinations by healthcare professionals specialized in diabetic foot care can identify early signs of problems. Prompt treatment of any detected issues can prevent progression. Patients should also seek immediate care if they experience pain, numbness, or new wounds.
Blood Sugar Control
Effective management of blood glucose levels through diet, medication, and lifestyle changes is fundamental in preventing nerve damage and vascular issues. Keeping blood sugar within target ranges significantly reduces the risk of foot complications.
Exercise and Circulatory Health
Engaging in gentle exercises like walking, toe stretches, and foot rotations can improve blood flow to the extremities. Regular movement helps maintain circulation, which is vital for tissue health and healing.
Medical Interventions for Advanced Foot Issues
Despite preventive measures, some diabetics may develop severe foot problems requiring medical treatment. These include debridement of infected tissue, antibiotic therapy for infections, and offloading techniques to reduce pressure on ulcers.
In more severe cases, surgical procedures such as amputations become necessary to prevent the spread of infection and save a patient’s life. Multidisciplinary teams comprising podiatrists, endocrinologists, and surgeons are involved in comprehensive diabetic foot management.
Final Thoughts
Diabetic foot complications can be life-altering and potentially limb-threatening if not detected early. Maintaining strict blood sugar control, practicing diligent foot care routines, wearing suitable footwear, and seeking regular medical assessments are critical strategies for preserving foot health. Education about the risks and proactive management can enable diabetics to lead active, healthy lives without the burden of preventable foot problems.