Comprehensive Strategies for Managing Hiatal Hernia: Treatments, Medications, and Lifestyle Tips
This comprehensive article explores the causes, symptoms, and treatment options for hiatal hernia, including medications, lifestyle changes, and surgical procedures. It emphasizes timely diagnosis and personalized management strategies to ensure effective relief and prevent complications. Suitable for patients and healthcare providers alike, the guide aids in understanding the condition and making informed decisions for optimal health outcomes.
Effective Approaches to Treating and Managing Hiatal Hernia
A hernia is a medical condition where an internal organ or part of it protrudes through an opening or weak spot in the surrounding muscle or tissue. Specifically, a hiatal hernia involves the upward movement of a part of the stomach into the chest cavity by passing through the esophageal hiatus of the diaphragm, a muscular structure separating the chest and abdominal regions. This condition predominantly affects individuals over the age of 50 but can occur at any age. Understanding the causes, symptoms, and treatment options for hiatal hernia is essential for effective management and quality of life preservation.
Understanding the Causes of Hiatal Hernia
The exact etiology of hiatal hernias remains uncertain; however, several factors are recognized as contributors. Increased pressure on the abdomen from activities such as coughing, vomiting, heavy lifting, or straining during bowel movements can push the stomach upward. Structural factors like an inherently large esophageal hiatus or weak diaphragmatic muscles predispose individuals to hernia development. Additional risk factors include obesity, advancing age, smoking habits, and conditions causing increased intra-abdominal pressure. These elements can weaken the supportive tissues of the diaphragm, allowing the stomach to herniate into the chest cavity.
Most individuals with hiatal hernia experience mild or no symptoms; however, some may encounter discomfort that affects daily activities. Common symptoms include frequent belching, a sensation of chest fullness, persistent heartburn that worsens when lying down or bending over, and difficulty swallowing. Recognizing these signs early can lead to prompt treatment and better outcomes.
While many cases are asymptomatic or involve mild discomfort requiring minimal intervention, persistent or severe symptoms necessitate medical attention. The management of hiatal hernia encompasses a combination of medications, lifestyle modifications, and surgical interventions designed to alleviate symptoms, promote healing, and prevent complications.
Antacids – Over-the-counter medications such as Mylanta, Tums, Rolaids, Gelusil, and Maalox provide quick relief by neutralizing excess stomach acid. They are often the first line of defense for mild symptoms.
Prescription Medications – H-2 receptor antagonists like ranitidine, famotidine, nizatidine, and cimetidine help reduce acid secretion, easing esophageal irritation. These are suitable for moderate to severe cases under medical supervision.
Proton Pump Inhibitors (PPIs) – Drugs such as omeprazole, lansoprazole, pantoprazole, and esomeprazole block acid production more effectively, promoting healing of the esophageal lining and reducing reflux symptoms.
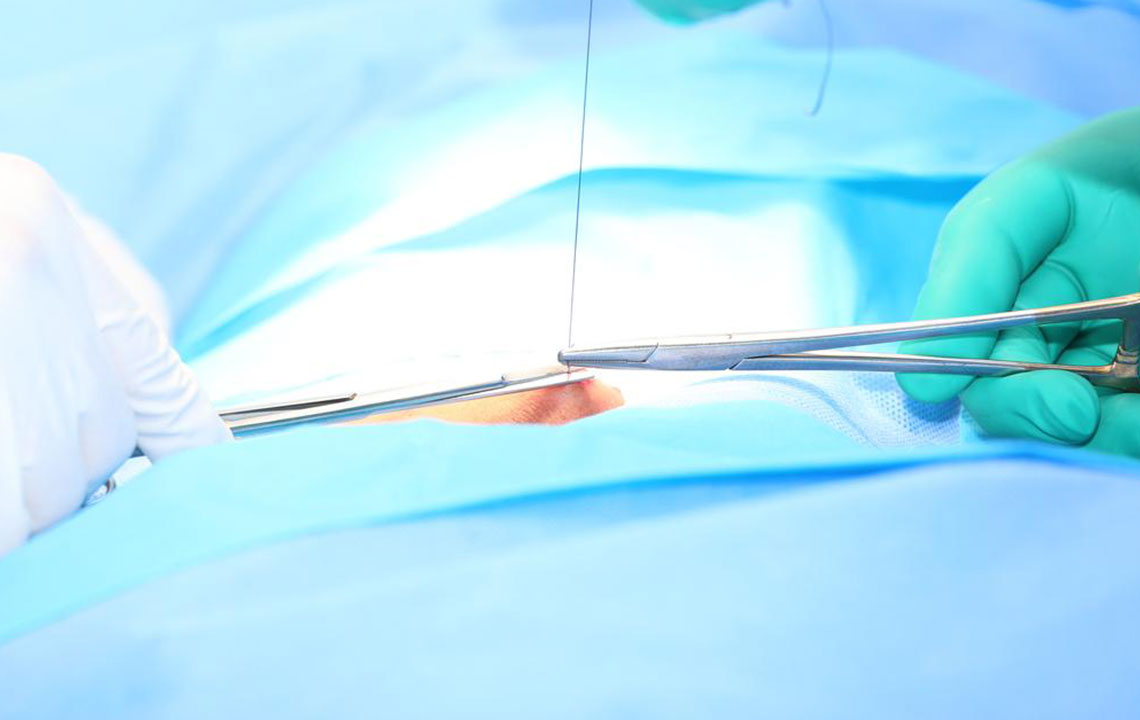
Surgical Options – When medications and lifestyle changes fail to control symptoms or complications arise, surgical intervention becomes necessary. Procedures involve repairing the hiatal defect, repositioning the stomach, and reinforcing the esophageal sphincter. Most surgeries are minimally invasive laparoscopic procedures with rapid recovery times. Techniques include Nissen fundoplication, Toupet fundoplication, and Belsey procedures, tailored to individual needs.
Postoperative recovery typically involves a brief hospital stay, usually 2-3 hours under general anesthesia, followed by a structured diet and activity plan. Although surgery can provide long-term relief, recurrence remains a possibility, emphasizing the importance of ongoing management. Besides surgical measures, lifestyle modifications play a crucial role in preventing hernia progression and alleviating symptoms.
Key lifestyle recommendations include maintaining a healthy weight, eating smaller and more frequent meals, avoiding spicy or acidic foods, elevating the head of the bed during sleep, and quitting smoking. These adjustments reduce intra-abdominal pressure and support the healing process. Additionally, avoiding tight clothing and strenuous activity can help manage symptoms effectively.
Other surgical techniques, such as the Belsey or Belsey-Mark IV procedure, are employed in specific cases. Patients should always consult qualified healthcare professionals for personalized treatment planning. Beware of unverified or unproven treatments, and focus on evidence-based approaches for optimal results.
In conclusion, proper management of hiatal hernia involves a multifaceted approach combining medications, lifestyle modifications, and surgical options when necessary. Early diagnosis and tailored treatment strategies help prevent complications like gastroesophageal reflux disease (GERD), esophageal ulcers, or severe discomfort, ultimately improving patient outcomes and quality of life.





