Comprehensive Guide to Obesity Evaluation with BMI Metrics
This comprehensive guide explores how BMI is used to assess obesity risk, including its calculation, classifications, limitations, and relevance for children. It emphasizes the importance of combining BMI with other health assessments for accurate diagnosis and effective weight management strategies. Understanding BMI helps individuals and health professionals better identify obesity-related health risks and promotes healthier lifestyles through balanced diets and regular exercise.
Comprehensive Guide to Obesity Evaluation with BMI Metrics
Obesity has become one of the most pressing health concerns worldwide, characterized by an excessive accumulation of body fat that significantly compromises overall health and well-being. The prevalence of obesity continues to rise at an alarming rate, with current statistics indicating that more than two-thirds of adults globally are affected. Even among children, the incidence of obesity is increasing, raising concerns about future health complications and lifetime health risks. This epidemic is driven by a combination of factors such as unhealthy dietary habits, sedentary lifestyles, genetic predispositions, and socio-economic influences. Recognizing and accurately assessing obesity is crucial for implementing effective intervention strategies to prevent associated health issues.
Obesity is linked to a heightened risk of developing multiple serious health conditions, including various forms of cancer, cardiovascular diseases such as hypertension and heart attacks, type 2 diabetes, and even early mortality. Because of its widespread impact, healthcare professionals and individuals alike prioritize early detection and assessment of obesity levels. Among the tools widely adopted for this purpose is the Body Mass Index (BMI) calculator, a simple yet effective method for quick obesity assessment.
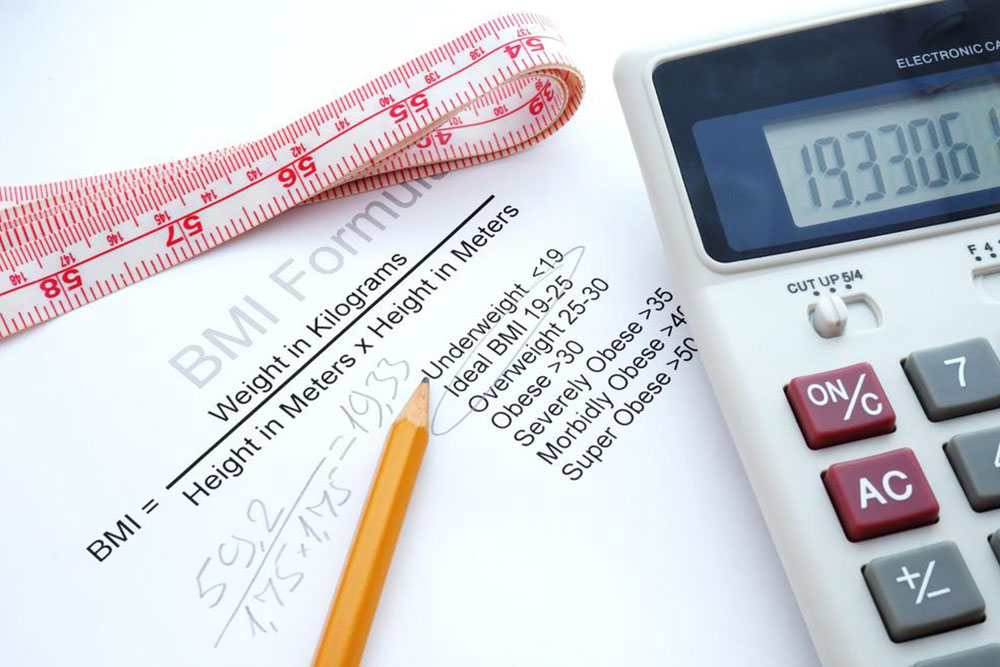
The BMI calculator operates by providing a straightforward numerical value derived from a person's height and weight, simplifying the process for both clinicians and individuals to evaluate body composition. This method offers a rapid, non-invasive, and inexpensive way to identify health risks related to weight.
The Body Mass Index, or BMI, is calculated by dividing an individual's weight in kilograms by the square of their height in meters. This calculation provides a single, standardized measure that allows health professionals to categorize individuals based on their weight status. The World Health Organization (WHO), since the 1980s, has adopted BMI thresholds as a global standard to monitor obesity prevalence and assess individual health risks. The BMI classifications are as follows:
BMI less than 18.5: Underweight
BMI between 18.5 and 24.9: Normal weight (healthy)
BMI between 25 and 29.9: Overweight
BMI of 30 or above: Obese
BMI exceeding 40: Severe or morbid obesity
Despite its simplicity and widespread use, BMI does have certain limitations. It does not account for variations in body composition, such as muscle mass, bone structure, or fat distribution. For example, athletes with high muscle mass may have elevated BMI readings but low body fat levels, potentially leading to misclassification. Conversely, individuals with normal BMI might carry excessive abdominal fat, which poses significant health risks even if their BMI appears within a healthy range. Therefore, BMI is most effective when used alongside other measures and clinical assessments.
Special Considerations for Children
For pediatric populations, BMI calculations follow a similar formula but are interpreted differently. Instead of fixed thresholds, BMI percentiles based on age and sex are used to determine weight status. This approach provides a more accurate assessment of growth patterns and body composition in children and teenagers. Common interpretative categories include:
Below the 5th percentile: Underweight
85th to 95th percentile: Overweight
Above the 95th percentile: Obese
Recent updates by WHO and other health authorities have revised BMI cut-offs and percentile thresholds, reflecting better understanding of pediatric growth patterns and health risks. Notably, in some regions, the BMI threshold for overweight shifted from 27.8 to 25, reclassifying many adults from the healthy weight category to overweight. Current surveys reveal that approximately 38% of adults are classified as obese, with women experiencing slightly higher rates than men. Severe obesity remains a significant public health challenge, affecting a considerable segment of the population and increasing the burden on healthcare systems.
Limitations of BMI as an Assessment Tool
While BMI provides a useful initial screening tool, it has notable limitations that necessitate supplementary assessment methods for comprehensive obesity evaluation. Since BMI is solely based on weight and height, it does not differentiate between lean muscle mass and fat tissue. Variations in body frame size can lead to misclassification — smaller-framed individuals with high fat content may be labeled as overweight or obese, while larger-framed individuals with low fat levels might appear to have a healthy BMI. Furthermore, BMI does not specify fat distribution, which is a critical factor since visceral fat, especially abdominal fat, is associated with higher risks of type 2 diabetes, heart disease, and metabolic syndrome.
Another challenge is that BMI does not account for differences in age, ethnicity, or gender, which influence body composition. For athletes and highly active individuals, elevated BMI values often reflect increased muscle mass rather than excess fat, potentially leading to inaccurate health risk assessments. Many research findings indicate that a significant number of individuals classified as overweight or obese based solely on BMI might not exhibit corresponding health risks. As such, clinical assessments often incorporate measurements like waist circumference, body fat percentage via calipers or imaging, and additional health markers to form a comprehensive picture.
Obesity is a multifaceted health issue that extends beyond mere numbers. It impacts psychological self-esteem, social interactions, and overall quality of life. Successfully combating obesity involves lifestyle changes reinforced by sustained motivation and support. Regular physical activity, combined with balanced, nutritious diets, promotes calorie expenditure and helps regulate weight. Behavior modification, counseling, and community support further enhance efforts to achieve and maintain healthy body weight.
While BMI calculators serve as valuable screening tools, they should be viewed as a starting point. A full obesity assessment involves a combination of clinical observations, lifestyle evaluation, and, when necessary, diagnostic tests. Adopting an active lifestyle, engaging in consistent fitness routines, and making healthy dietary choices are fundamental strategies for maintaining a healthy weight and reducing health risks. Recognizing the complex nature of obesity and approaching it with comprehensive strategies are essential for effective prevention and treatment.