Comprehensive Guide to Women's Heart Health: Key Insights and Preventive Measures
This comprehensive guide explores essential insights into women's heart health, highlighting unique symptoms, risk factors, and preventive strategies. Emphasizing the importance of early detection and tailored care, it aims to empower women and healthcare providers to combat rising heart disease rates and improve outcomes through informed decision-making and proactive health management.
Comprehensive Guide to Women's Heart Health: Key Insights and Preventive Measures
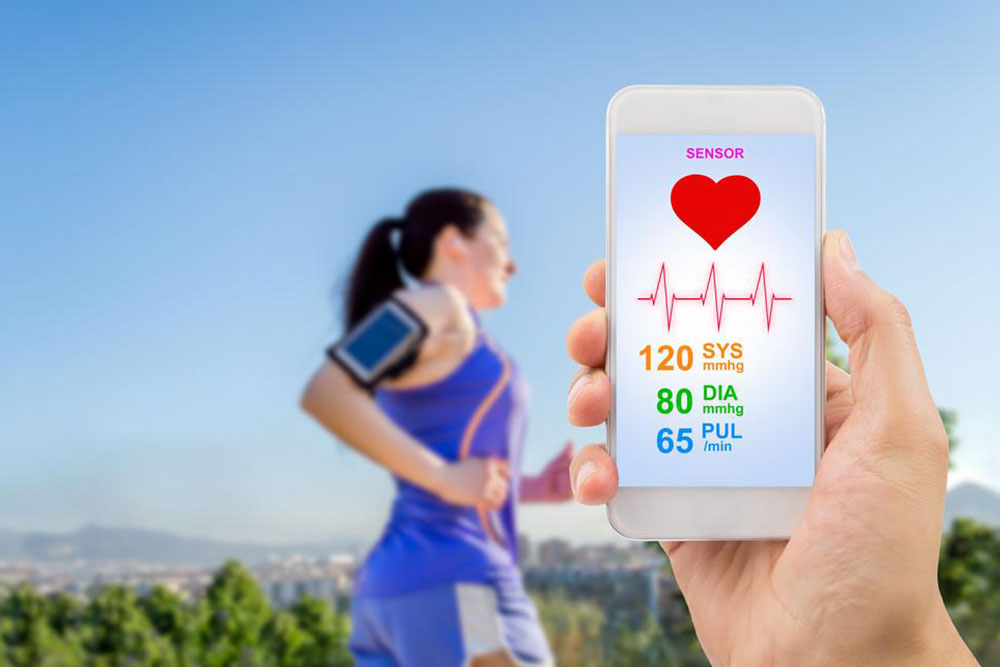
Maintaining optimal heart health is a critical aspect of overall well-being, especially for women, whose cardiovascular health needs often differ significantly from men's. Despite increased awareness, many women remain unaware of specific risk factors, subtle symptoms, and the unique ways heart disease manifests in females. Understanding these differences, recognizing early warning signs, and adopting effective preventive strategies are vital steps toward reducing the incidence of heart-related illnesses and improving quality of life.
Cardiovascular disease remains the leading cause of death among women worldwide. According to recent studies, factors such as chronic stress, anxiety, high blood pressure, abnormal cholesterol levels, and hypertension significantly elevate the risk of developing heart problems. However, the way these factors influence women’s health differs from men due to anatomical, hormonal, and physiological variations, making targeted research and tailored healthcare approaches essential.
Understanding women's heart health involves recognizing specific aspects that set it apart. Here are some crucial insights that can guide women and healthcare providers in proactive heart disease management:
The subtle presentation of symptoms: Unlike men, women often experience less dramatic symptoms during a cardiac event. Early signs can be mild and easily mistaken for anxiety or other benign conditions. Common early indicators include unexplained fatigue, shortness of breath, chest discomfort, stress, anxiety, and discomfort below the left shoulder blade. These subtler symptoms often delay diagnosis because they are less recognized as signs of heart trouble.
Long-term implications: The impact of untreated or unnoticed heart conditions tends to be more significant in women over time. Women are more prone to developing complications such as heart failure, arrhythmias, and even post-heart attack recovery challenges. Age-related deterioration compounds these risks, highlighting the importance of early detection and lifestyle modifications.
The influence of estrogen: Estrogen, a primary female hormone, plays a protective role by helping regulate cholesterol levels and maintaining the elasticity of blood vessels during reproductive years. However, after menopause, estrogen levels decline, leading to an increase in low-density lipoprotein (LDL or 'bad' cholesterol) and decreased high-density lipoprotein (HDL or 'good' cholesterol). This hormonal shift raises the risk of atherosclerosis and coronary artery disease in postmenopausal women.
Differences in heart anatomy: Women generally have smaller hearts and thinner arterial walls compared to men, making them more vulnerable to blockages caused by cholesterol buildup. Smaller coronary arteries can lead to increased incidences of microvascular disease, which affects the small vessels of the heart and can complicate diagnosis and treatment.
Understanding angina: Angina, a symptom of ischemic heart disease manifested as chest pain or discomfort, often presents differently in women. Unlike the intense, crushing chest pain often seen in men, women may experience a sensation of pressure, tightness, or burning that can be mistaken for gastrointestinal issues, such as acid reflux or indigestion. Recognizing these differences is crucial for timely medical intervention.
Preventive measures tailored specifically for women include regular cardiovascular screenings, maintaining a balanced diet, engaging in physical activity, managing stress, and avoiding smoking and excessive alcohol consumption. Additionally, hormone replacement therapy (HRT) may be discussed with healthcare providers to address hormonal changes after menopause, though its benefits and risks should be carefully weighed.
In conclusion, women’s heart health requires heightened awareness and personalized healthcare strategies that account for their unique physiological and hormonal profiles. Early detection, lifestyle modifications, and targeted treatment can significantly reduce the burden of heart disease in women, ultimately saving lives and enhancing quality of life.





