Effective Strategies for Managing Low Testosterone Levels in Men
Explore comprehensive strategies to manage low testosterone levels in men, including symptoms, causes, and various testosterone replacement therapies. This detailed guide helps men understand when and how to seek effective treatment options to improve their health and quality of life, emphasizing personalized approaches and medical supervision for safe and effective management.

Comprehensive Approaches to Address Low Testosterone in Men
Testosterone, a crucial hormone produced primarily in the testes, plays an indispensable role in the development and maintenance of male characteristics. It is responsible for the growth of facial and body hair, deepening of the voice during puberty, and increased muscle mass. Beyond these physical attributes, testosterone also influences vital bodily functions including red blood cell production, maintaining strong bone density, regulating mood, and supporting cognitive functions. Understanding the dynamics of testosterone levels is essential for men experiencing symptoms associated with decline, especially aging-related drops that typically begin after the age of 40.
In early adulthood, testosterone levels reach their peak, facilitating various physical and mental functions. However, after 40, levels tend to gradually decrease, which can lead to a host of symptoms affecting quality of life. Men over 50 are particularly susceptible to manifestations like diminished libido, erectile dysfunction, fatigue, weight gain, reduced muscle strength, and anemia—conditions directly linked to declining testosterone levels.
While age naturally influences hormone levels, a variety of other factors can contribute to low testosterone. These include medical issues such as infections, physical injuries to the testes, cancer treatments like chemotherapy and radiation, long-term use of steroids, chronic stress, obesity, excessive alcohol consumption, and serious illnesses. Normal testosterone levels in the bloodstream are generally considered to be between 300 and 1000 nanograms per deciliter (ng/dL). Levels below this range are indicative of hypogonadism or testosterone deficiency, which warrants medical attention. Recognizing symptoms early and consulting healthcare professionals are critical steps toward effective management and treatment.
Age-related decrease in testosterone is common; however, low testosterone levels caused by underlying health conditions require targeted interventions. Not all men with low levels need treatment—clinical evaluations focus on the severity of symptoms and underlying causes. Conditions such as excessive weight gain, thyroid dysfunction, or side effects from medications are primary considerations for therapy. When men exhibit symptoms like persistent fatigue, low libido, and muscle weakness, comprehensive health assessments are conducted, including evaluations of bone density, prostate health, kidney function, and cardiovascular risk factors. For men with osteoporosis or low bone density, testosterone therapy may be beneficial, whereas those with prostate enlargement or heart issues are usually advised to avoid such treatment due to potential risks.
Understanding Testosterone Replacement Therapy (TRT)
The cornerstone of medical intervention for low testosterone is hormone replacement therapy (TRT), designed to restore hormone levels to the normal range and alleviate associated symptoms. This therapy can significantly improve quality of life when appropriately administered and monitored by healthcare providers. Various delivery methods are available, allowing for personalized treatment plans based on patient needs and preferences:
Intramuscular injections
Topical gels or skin patches
Mouth patches or buccal tablets
Subcutaneous pellet implants
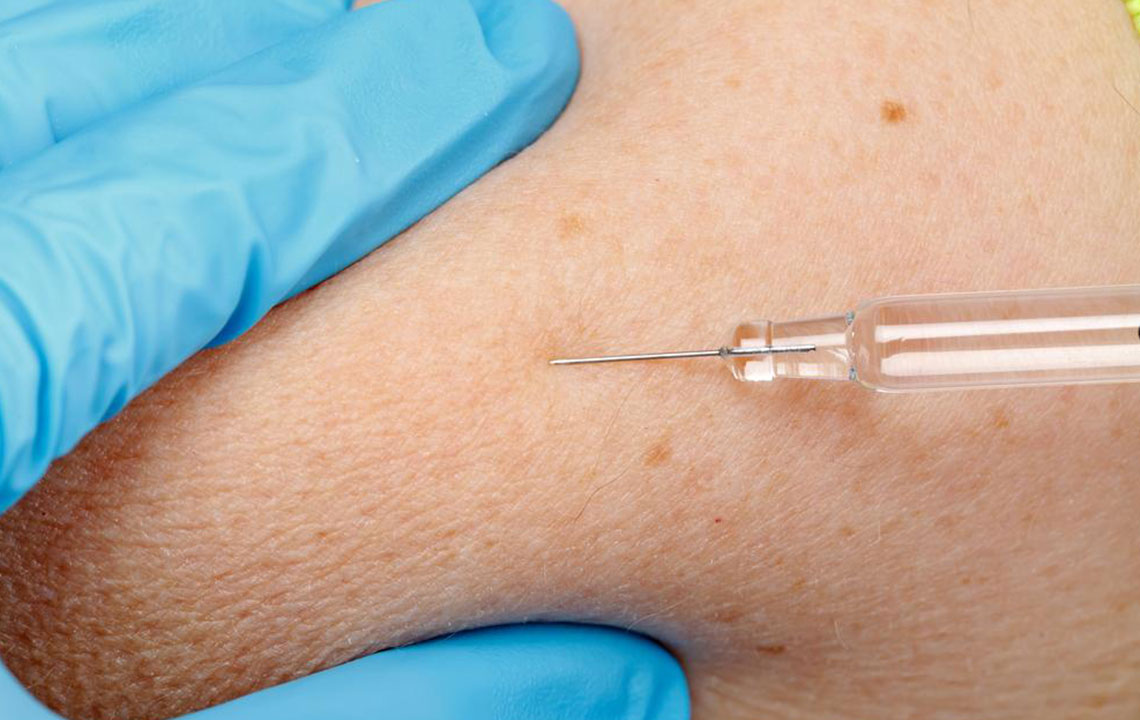
Intramuscular Injections
This method involves injecting testosterone directly into the muscle. It is cost-effective and typically administered every 7 to 14 days, depending on dosage. Patients often experience a rapid increase in hormone levels, providing quick symptom relief. However, injections can be uncomfortable, and some men may encounter mood swings or energy fluctuations as hormone levels stabilize.
Topical Gels and Patches
Applied once daily on clean, dry skin, these products provide a steady release of testosterone, mimicking natural fluctuations. This method is convenient and painless, making it popular among patients. Nevertheless, careful application is necessary to prevent skin irritation or allergic reactions. Additionally, it is critical to avoid contact between the treated area and other people—especially women and children—to prevent accidental exposure to testosterone.
Mouth Patches and Buccal Tablets
Placed inside the cheek or gum twice daily, these devices allow testosterone to be absorbed through the oral mucosa. Buccal patches do not interfere with eating or drinking and provide a consistent hormone level. Possible side effects include oral irritation or an unpleasant taste, but they are generally well-tolerated.
Pellet Implants
Subcutaneous pellets inserted into the hip or buttocks provide long-lasting testosterone delivery, usually between 3 to 6 months. These implants release hormone gradually, ensuring stable blood levels. Patients typically notice improvements in mood, energy, and muscle mass within 4 to 6 weeks. It is essential that this treatment be regularly monitored by healthcare professionals to assess efficacy and detect any potential side effects or complications.
Overall, the decision to pursue testosterone replacement therapy should involve a thorough discussion with a healthcare provider, considering the potential benefits, risks, and individual health profile. It is crucial to conduct regular follow-ups and blood tests to adjust the treatment plan as needed, ensuring safety and optimal results.