Comprehensive Guide to Skin Cancer: Types, Symptoms, and Effective Treatment Strategies
This comprehensive article provides an in-depth overview of skin cancer, including its various types, symptoms, risk factors, diagnostic methods, and treatment options. It emphasizes the importance of early detection and showcases advanced treatment strategies like Mohs surgery and targeted therapies. Perfect for those seeking detailed yet accessible information about skin cancer to promote awareness and timely intervention.
Comprehensive Guide to Skin Cancer: Types, Symptoms, and Effective Treatment Strategies
Skin cancer is one of the most common forms of cancer worldwide, with millions of new cases diagnosed each year. Originating from the epithelial tissues of the skin, this disease can manifest on the surface of the skin or internally, affecting organs such as the liver, kidneys, and more. Understanding the various types of skin cancer, their symptoms, risk factors, and available treatment options is crucial for early diagnosis and effective management. Due to its prevalence and potential severity, especially if diagnosed late or left untreated, being informed about skin cancer is vital for anyone concerned about skin health and overall wellbeing.
Different Types of Skin Carcinomas
Skin carcinomas are classified based on the type of skin cells they originate from. These classifications help medical professionals determine prognosis, treatment options, and likely outcomes. Sometimes, multiple types of carcinomas may develop simultaneously in the same region, complicating diagnosis and management. Here, we explore the most common subtypes of skin cancer, their characteristics, and implications.Common skin cancer subtypes include:
Basal Cell Carcinoma (BCC): This is the most prevalent type of skin cancer, accounting for the majority of non-melanoma skin cancers. BCC tends to grow slowly and rarely metastasizes to other parts of the body. It primarily develops on sun-exposed areas such as the face, neck, and ears. Excessive ultraviolet (UV) radiation from sun exposure or tanning beds is the biggest risk factor. BCC often appears as a shiny, translucent bump that may look like a sore that doesn’t heal, or as a waxy, flesh-colored lesion. It can sometimes form a crater or ulcerate, especially if left untreated. Early detection and treatment are crucial to prevent local tissue destruction and cosmetic disfigurement.
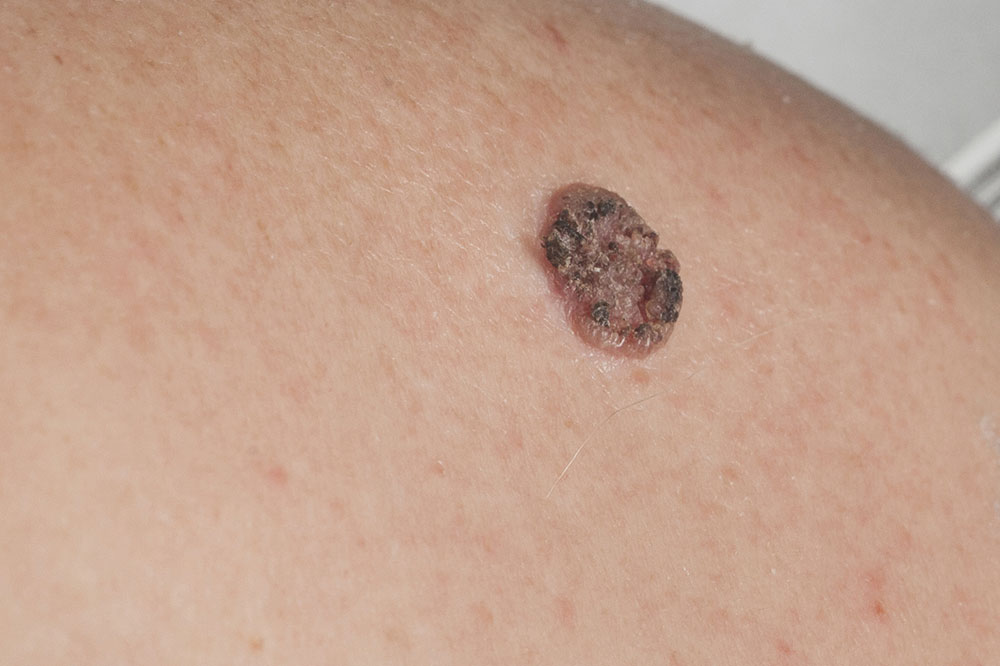
Squamous Cell Carcinoma (SCC): The second most common skin cancer, SCC, can also develop on sun-exposed skin but has a higher tendency to invade deeper tissues and metastasize compared to BCC. It often presents as a rough, red, scaly bump or a sore that persists and may bleed or crust over. Like BCC, SCC is strongly associated with UV exposure, and risk factors include fair skin, chronic sun damage, and immunosuppression. While it more frequently affects areas such as the hands, arms, face, and ears, SCC can also affect internal organs if it metastasizes. Timely intervention is vital to prevent invasive growth.
Merkel Cell Carcinoma: A rarer but highly aggressive skin cancer, Merkel cell carcinoma usually appears as a rapidly growing, firm, flesh-colored or bluish lesion, typically on sun-exposed skin like the face and neck. It can metastasize quickly, making early diagnosis and prompt treatment essential. Unlike BCC and SCC, it tends to grow rapidly and requires aggressive treatment such as surgery combined with radiation or immunotherapy.
Kidney Cancer (Renal Cell Carcinoma): Although primarily a kidney disease, some kidney tumors—specifically renal cell carcinomas—can present as skin metastases in advanced stages. These tumors tend to form a solitary mass within the kidney but may spread through the bloodstream or lymphatic system to other organs, including the skin in rare cases.
Transitional Cell Carcinoma: Originates from the transitional epithelium lining the urinary tract, especially in the lining of renal pelvis, ureters, and bladder. It accounts for around 10% of kidney cancers and may sometimes metastasize to skin or present with secondary skin lesions in advanced cases.
Glandular Carcinomas (Adenocarcinomas): These originate from secretory epithelial cells and include several common cancers such as colorectal, pancreatic, prostate, breast, and lung cancers. Though not primary skin cancers, metastases from these types can sometimes manifest as skin nodules or lesions, especially in advanced stages.
After confirming diagnosis, skin carcinomas are further classified based on their extent and spread:
Carcinoma in situ: Confined to the original epithelial layer, without invading deeper tissues. This early stage is often curable with localized treatment.
Invasive carcinoma: Has penetrated beyond the epithelial layer into surrounding tissues, requiring more aggressive treatment approaches.
Metastatic carcinoma: Has spread from the primary site to distant parts of the body, including skin, and often indicates advanced disease requiring systemic therapy.
Recognizing the Signs and Symptoms of Skin Cancer
Being vigilant about skin changes is vital for early detection. Regular self-examinations can help spot suspicious lesions or changes in skin appearance. Skin cancers often begin as new growths, sores that don’t heal, or existing moles that change in size, shape, or color. They may bleed, crust, or become painful as they progress. Because early-stage cancers are often visible and accessible, prompt medical assessment markedly improves outcomes. It’s important to note that some skin cancers may resemble benign skin conditions, which is why professional evaluation is essential.Specific symptoms vary depending on the carcinoma type:
Basal Cell Carcinoma: Typically appears as a shiny, pale or translucent bump with blood vessels visible at its center. It may resemble a scar or flesh-colored bump and may bleed or crust over time if left untreated.
Squamous Cell Carcinoma: Usually manifests as a rough, scaly, red patch or nodule that does not heal after several weeks. It often occurs on sun-exposed areas such as the face, ears, neck, and hands, gradually enlarging if untreated.
Merkel Cell Carcinoma: Presents as a rapidly enlarging, firm, flesh-colored or bluish nodule. Given its aggressive nature, early detection is critical for better prognosis.
Causes and Established Risk Factors
UV radiation remains the primary culprit behind most skin cancers. Prolonged exposure to UV rays from the sun or artificial sources like tanning beds increases the risk of DNA damage in skin cells, leading to abnormal growth. Overexposure to UV light can cause mutations in the genes regulating cell growth, resulting in uncontrolled proliferation. Other significant risk factors include light skin, freckles, numerous moles, family history of skin cancer, and immunosuppressive conditions. Certain inherited syndromes, autoimmune diseases, and exposure to carcinogenic chemicals further heighten the risk. Precancerous lesions such as actinic keratosis are known precursors, signaling increased vulnerability. Chronic injury from burns, X-ray radiation, or chemical exposure can also contribute to specific types of skin cancer like squamous cell carcinoma.Diagnosing Skin Cancer Effectively
Diagnosis begins with a comprehensive physical examination by a qualified dermatologist, who assesses the shape, size, color, and texture of suspicious lesions. High-resolution photography might be used to monitor changes over time. A detailed medical history, including sun exposure habits, family history, and previous skin issues, provides additional clues. The most definitive step is a biopsy, where a small tissue sample is examined microscopically to confirm whether the lesion is malignant or benign. Biopsies can be performed in various ways, such as shave, punch, or excisional biopsy, depending on lesion characteristics.Prominent Treatment Strategies
Treatment choice depends on the type, size, location, and stage of the cancer, as well as the patient’s overall health. A multidisciplinary team comprising dermatologists, oncologists, and surgeons collaborates to develop the most suitable approach. Common methods include:
Electrodesiccation and Curettage: Suitable for small, superficial lesions, involving scraping off the tumor followed by cauterization to destroy remaining cells.
Surgical Excision and Mohs Micrographic Surgery: Frequently used for larger or recurrent lesions. Mohs surgery offers the highest cure rate by removing the tumor layer by layer and examining each under the microscope in real-time, preserving healthy tissue.
Cryosurgery: Involves freezing cancer cells with liquid nitrogen, leading to cell death. Ideal for superficial BCC and SCC.
Topical Chemotherapy: Application of medicated creams or gels like 5-fluorouracil or imiquimod directly onto the lesion. This minimally invasive option is suitable for superficial lesions.
Radiation Therapy: Targeted high-energy radiation treats tumors that are difficult to remove surgically or in patients unable to undergo surgery.
Laser Therapy: Uses concentrated light beams to vaporize or destroy superficial cancerous tissue with precision.
In addition to these options, emerging treatments such as immunotherapy are showing promise, especially for advanced or metastatic skin cancers. Early detection and tailored treatment strategies significantly improve survival rates and quality of life for patients.




