A Comprehensive Guide to Blood Donation: Types, Compatibility, and Process
This comprehensive guide explores the importance of blood donation, explaining the types of donations, blood compatibility systems like ABO and Rh factors, and the donation process. It emphasizes the critical role of donors in saving lives and highlights key eligibility requirements. Whether you're interested in donating whole blood, plasma, platelets, or double red cells, this article provides detailed information to help you understand how blood donation can make a difference for patients in need around the world.

Understanding Blood Donation: Essential Information and Types
Blood donation is one of the most vital acts that save lives and support healthcare systems worldwide. Every day, millions of patients rely on the generosity of donors to receive life-saving transfusions. In the United States alone, blood is needed every 2 seconds to meet ongoing medical demands. The significance of blood donation becomes even more apparent when considering that many transfusions are administered to vulnerable populations, especially children under the age of five in developing regions. Patients battling chronic illnesses such as cancer, sickle cell anemia, and traumatic injuries depend heavily on blood transfusions to survive and recover. This comprehensive guide explores the importance of blood donation, different types of donations, blood group systems, compatibility considerations, and the process involved in donating blood, ensuring donors are well-informed and prepared for their life-saving acts.
Understanding Blood Classification Systems
ABO Blood Group System
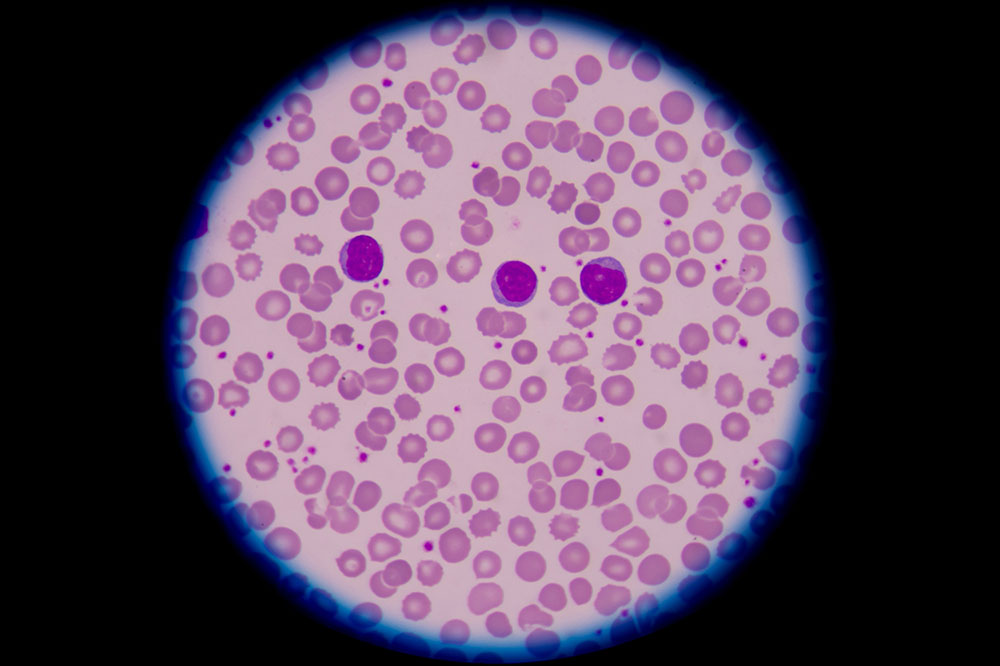
Blood classification is essential to ensure safe and effective transfusions. The most widely recognized system is the ABO blood group system, which categorizes blood into four primary groups: A, B, O, and AB. This classification hinges on the presence or absence of specific sugars, called antigens, on the surface of red blood cells. These antigens are vital for compatibility because the immune system produces antibodies against foreign antigens, which can cause dangerous transfusion reactions if mismatched. For instance, individuals with type A blood have A antigens and produce anti-B antibodies, while type B individuals have B antigens and produce anti-A antibodies. Those with type AB have both A and B antigens and can accept all blood types—hence, they are called universal recipients. Conversely, type O blood does not carry A or B antigens, making it the universal donor, suitable for transfusing into any blood type. In the U.S., approximately 42% of the population has type A blood, 10% has B, 44% have O, and 4% possess AB blood. These percentages can vary regionally and ethnically but highlighting the core importance of blood type compatibility in transfusions.
Rh Factor and Its Role in Transfusions
The Rh factor is another critical component influencing blood compatibility. It is a specific protein found on the surface of red blood cells. Blood is classified as Rh-positive if the Rh antigen is present, and Rh-negative if it is absent. Rh-positive blood is more prevalent, especially in the United States, where the most common blood types are O+ and A+. The significance of Rh compatibility is paramount during transfusions because mismatched Rh can lead to hemolytic reactions, which are serious immune responses where the recipient's immune system attacks the transfused red blood cells. For example, an Rh-negative individual receiving Rh-positive blood may develop anti-Rh antibodies, leading to complications in future transfusions or pregnancies. Therefore, blood compatibility testing includes ABO and Rh typing to prevent adverse reactions and ensure donor-recipient safety.
Additional blood antigens exist beyond ABO and Rh, but they are less frequently involved in transfusion compatibility. Ensuring compatibility between donor and recipient blood types is essential to avoid potentially life-threatening reactions. Medical professionals perform meticulous testing before administering any transfusion to confirm the safety of the procedure.
Different Types of Blood Donations
Blood donation isn’t a one-size-fits-all process; there are several types of donations tailored to meet different medical needs. These include traditional whole blood donation, plasma donation, platelet donation, double red cell donation, as well as autologous and directed donations. Each type has specific procedures, uses, and donor eligibility requirements, making it possible to address diverse patient conditions effectively.
Whole Blood Donation
Whole blood donation involves collecting a sample that contains all critical components: red blood cells, white blood cells, plasma, and platelets. The primary purpose of whole blood donation is to provide a versatile supply that can be separated into individual components and used to help multiple patients. Red blood cells are the most frequently used component as they carry oxygen throughout the body, vital for patients suffering from anemia or significant blood loss. White blood cells, which help fight infections, and platelets, essential for clotting, are also valuable components, especially in trauma and cancer therapies. Plasma contains essential proteins, hormones, and clotting factors, making it another critical component for treating clotting disorders, burn victims, and immune deficiencies. A standard whole blood donation takes approximately one hour, including health screening, and allows donors to give every 8 weeks.
Plasma Donation and Collection
Plasma is the yellowish, straw-colored part of blood that contains vital proteins, hormones, and clotting factors. It is crucial for managing conditions such as hemophilia, immune deficiencies, and severe burns. Unlike whole blood donation, plasma donation uses a process called plasmapheresis, where blood is drawn from the donor, and the plasma is separated and collected via a specialized machine. The remaining blood components, such as red blood cells and white blood cells, are then returned to the donor’s body. This process typically takes about 1.5 to 2 hours. Plasma donations are generally permitted every 28 days, depending on health and local regulations. Donors with certain blood types, especially AB, can donate plasma more frequently because AB plasma is universal and in high demand.
Platelet Donation and Its Significance
Platelet donation is particularly crucial for patients suffering from bleeding disorders, cancer treatments, or severe injuries, as platelets are essential for blood clotting. Plateletpheresis, the process of collecting platelets, involves extracting these small cell fragments while returning other blood components to the donor. The procedure typically lasts about three hours and can be performed weekly. Donors are allowed to donate platelets up to 24 times annually, making it a sustainable way to support patients in urgent need of clotting factors.
Double Red Cell Donation: Power Red
This type of donation, also known as double red cell donation, allows for the collection of a larger volume of red blood cells in a single session. Using a specialized machine, donors undergo a process that separates blood components and collects red cells while returning plasma and platelets. The procedure takes roughly 30 minutes longer than standard whole blood donation but yields a greater amount of red cells—an essential resource for patients with severe blood loss or anemia. Eligibility criteria include specific height and weight requirements to ensure safety, and donors can donate this type of blood every 16 weeks. Power Red donations are particularly valuable because they provide a concentrated dose of red cells needed for critical transfusions.
Specialized Blood Donations
In addition to the standard donation types, there are specific categories designed to meet particular needs or conditions. Autologous donations involve a donor collecting their own blood before planned surgery, reducing the risk of transfusion reactions. These donations can be made every few days under medical supervision, and the blood is stored for personal use. Directed donations are aimed at specific recipients, often family members or close friends, with special arrangements and pre-surgical planning. These types of donations ensure that the blood reaches the recipient in a timely and safe manner, especially during elective surgeries or in cases with known rare blood types.
Understanding the different donation methods and their purposes enables potential donors to choose the right type for their circumstances and helps healthcare providers meet diverse transfusion needs efficiently. Donors are encouraged to consult with local blood centers to ensure they meet eligibility criteria and to understand the donation process thoroughly, which is safe and beneficial for both donor and recipient.