Complete Guide to Managing and Treating Herniated Spinal Discs
This comprehensive guide explores herniated disc symptoms, causes, and effective treatment methods. From conservative therapies to surgical options, learn how to manage this common spinal condition. Early diagnosis is vital for preventing nerve damage and restoring mobility. Discover key strategies for pain relief, rehabilitation, and long-term prevention to improve quality of life and spinal health.
In-Depth Overview of Herniated Discs: Recognizing Symptoms, Understanding Causes, and Exploring Treatment Strategies
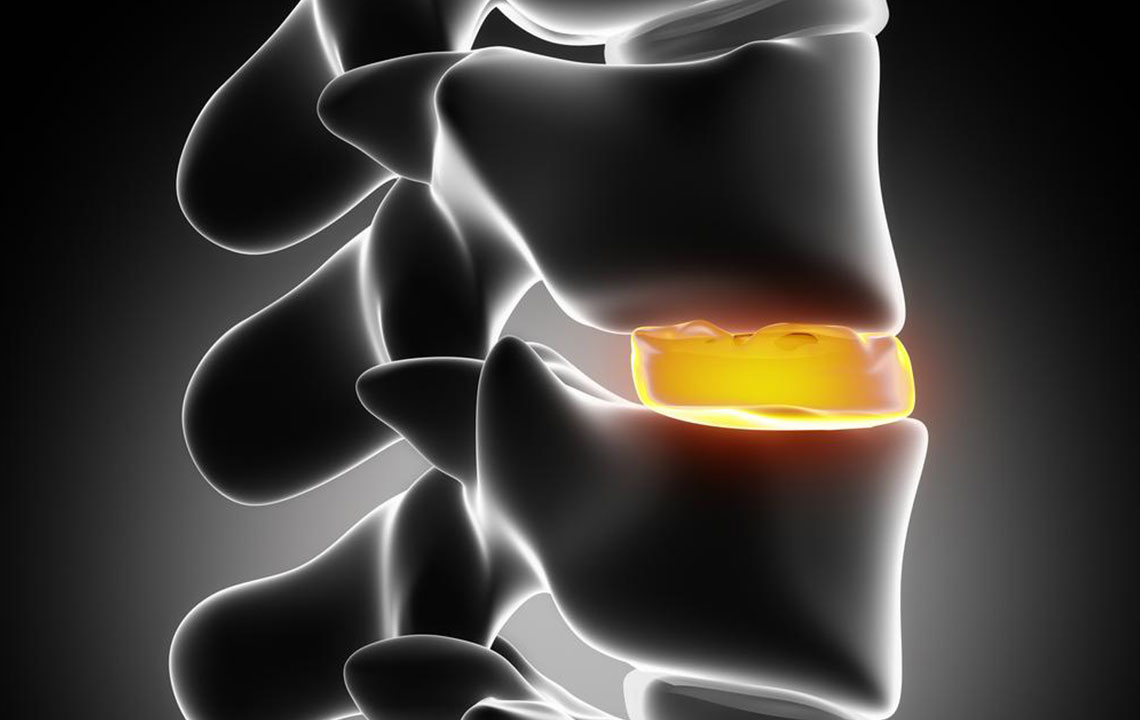
A herniated disc, commonly referred to as a slipped or ruptured disc, is a prevalent spinal condition that can significantly impact quality of life. It manifests through symptoms such as numbness, weakness, tingling sensations in the arms or legs, and sometimes severe pain. This condition arises when one of the intervertebral discs, which serve as cushions between the spinal vertebrae, protrudes beyond its normal boundary, exerting pressure on surrounding nerve structures. Such pressure can lead to neurological symptoms, discomfort, and mobility issues. Although a herniated disc may sometimes be painless, its potential to cause pain and neurological deficits makes understanding its management crucial.
Spinal discs are essential structures composed of glycoproteins and fibrocartilage, functioning as shock absorbers that provide cushioning and flexibility to the spine. Each disc has an outer fibrous layer called the annulus fibrosus and an inner gel-like core known as the nucleus pulposus. Damage or degeneration to the outer layer can allow internal disc material to bulge or herniate, pressing against neural tissues. Such damage can be triggered by various factors, including injuries, repetitive microtrauma, genetic predisposition, or age-related degeneration. When herniation occurs, symptoms depend on the affected area of the spine—cervical herniations tend to cause neck and arm symptoms, whereas lumbar herniations often result in lower back pain, sciatica, or leg weakness.
The causes of herniated discs are multifaceted. They include cumulative minor injuries over time, sudden traumatic events like falls or accidents, and hereditary factors that weaken spinal structures. Certain lifestyle choices, such as poor posture, lack of exercise, or overweight conditions, can exacerbate the risk. Symptoms can develop gradually or suddenly, often worsening with activities that increase pressure on the spine, such as bending, lifting, or prolonged sitting. In more severe cases, nerve compression can lead to bowel or bladder disturbances or even paralysis, making timely intervention essential.
Initial management of herniated discs primarily focuses on conservative, non-surgical approaches aimed at alleviating symptoms, reducing inflammation, and promoting natural healing. These methods include medication for pain relief, anti-inflammatory drugs, physical therapy, and lifestyle modifications. Physical therapy plays a significant role in restoring mobility, strengthening supportive muscles, and preventing further injury. The recovery process is often divided into four distinctive phases:
Phase 1: Pain Relief and Protective Measures - During this phase, the emphasis is on reducing inflammation and pain through the use of ice packs, medications such as NSAIDs, and alternative therapies like acupuncture. This phase also involves educating patients on activity modifications to prevent aggravation of symptoms.
Phase 2: Restoring Functionality - Focused on improving joint alignment, flexibility, and muscular stability through targeted exercises. Core strengthening routines, massage therapy, and gentle stretching help alleviate pressure on affected nerves and promote healing.
Phase 3: Achieving Full Motor Function - As symptoms improve, treatment shifts toward restoring full control over spinal movements, enhancing strength in the pelvis, back, and leg muscles. Activities are gradually intensified, progressing from walking to light exercise routines suitable to the patient’s capacity.
Phase 4: Preventive Strategies for Recurrence - The final phase centers on maintaining spinal health through personalized exercise routines, posture correction, ergonomic adjustments, and lifestyle modifications to minimize the risk of future herniation episodes.
While conservative treatment is effective for most cases, some patients may not respond adequately, necessitating surgical intervention. Surgical options vary based on the location and severity of the disc herniation. Common procedures include discectomy, microdiscectomy, or more advanced spinal fusion techniques. Early diagnosis and prompt treatment are critical to prevent long-term nerve damage, chronic pain, and functional impairment. With proper care, many individuals recover fully and return to their daily activities, underscoring the importance of medical intervention and individualized treatment planning for herniated disc management.





