Comprehensive Guide to Tardive Dyskinesia: Causes, Diagnosis, and Effective Management Strategies
This detailed guide explores the causes, diagnostic methods, and management strategies for tardive dyskinesia. Understanding the roots of this neurological disorder helps in early detection and better treatment. The article discusses the role of medications, lifestyle interventions, and advanced therapies like deep brain stimulation in managing symptoms and improving quality of life. It emphasizes the importance of regular monitoring and a multidisciplinary approach to care, especially for vulnerable populations. Early intervention and ongoing care are essential to reduce the impact of this challenging condition.

Comprehensive Guide to Tardive Dyskinesia: Causes, Diagnosis, and Effective Management Strategies
Tardive dyskinesia (TD) is a complex neurological disorder characterized by involuntary, repetitive movements that often affect the face, tongue, lips, and limbs. This condition can significantly impair daily functioning and quality of life if not properly managed. Understanding the origins, diagnostic procedures, and treatment options for TD is crucial for patients, caregivers, and healthcare providers. In this comprehensive guide, we delve into every aspect of tardive dyskinesia, including its underlying causes, how it is diagnosed, and the latest management strategies available to help mitigate its symptoms and improve patient well-being.
Understanding the root causes of tardive dyskinesia is essential for effective management. The primary cause is prolonged usage of certain medications, particularly neuroleptic and antipsychotic drugs, which interfere with dopamine—a critical neurotransmitter involved in regulating movement and reward pathways in the brain. While these medications are vital in treating psychiatric conditions such as schizophrenia and bipolar disorder, their long-term administration can lead to irreversible movement disorders like TD. Additional factors contributing to the development of TD include age-related changes, hormonal fluctuations such as menopause, and lifestyle factors like substance abuse. Recognizing these risk factors allows for better preventative measures and early interventions.
Diagnosing tardive dyskinesia can be challenging because its symptoms tend to develop gradually and may resemble other movement disorders such as Parkinson's disease or dystonia. Accurate diagnosis involves comprehensive clinical assessment using specialized tools such as the Abnormal Involuntary Movement Scale (AIMS), which evaluates the severity and distribution of involuntary movements. Furthermore, advanced imaging techniques, including MRI and PET scans, can help identify structural or functional brain changes associated with TD. Early detection is critical because it allows for timely intervention, which can reduce severity and prevent progression.
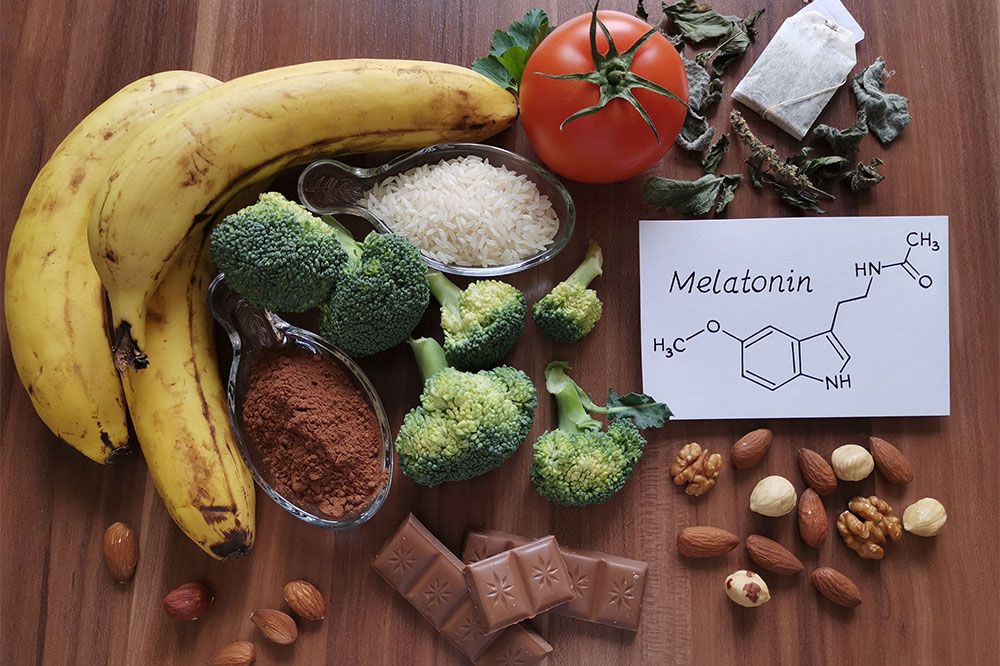
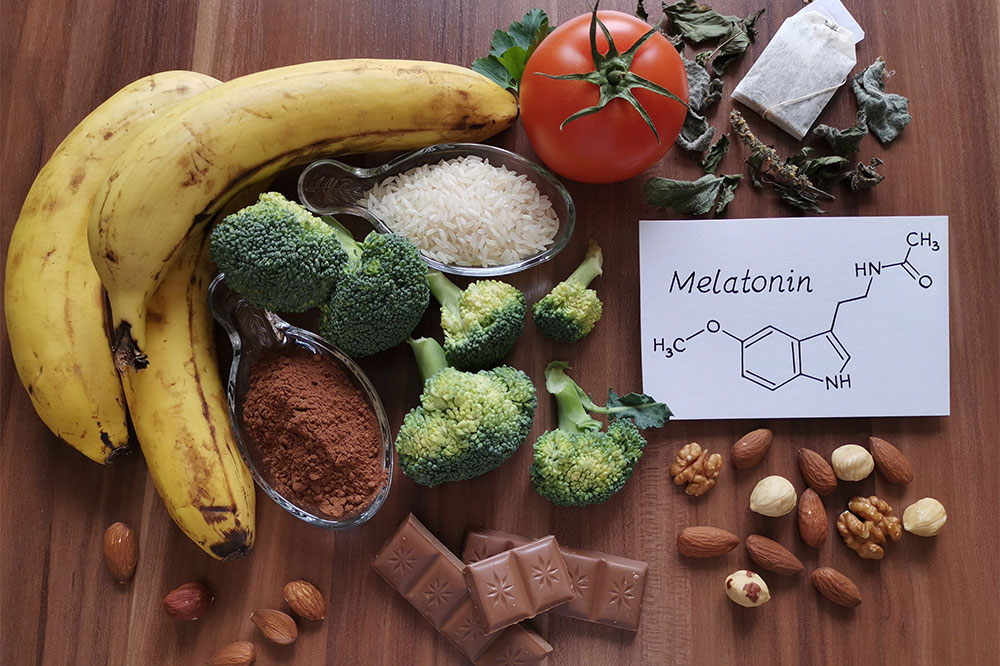
Although there is currently no definitive cure for tardive dyskinesia, various management options focus on alleviating symptoms, preventing complications, and improving patients' overall quality of life. Pharmacological adjustments are often the first step—this may involve reducing the dose of offending medications under medical supervision or switching to drugs with lower risk profiles. In addition, certain medications such as VMAT2 inhibitors (e.g., valbenazine and deutetrabenazine) have shown promise in reducing involuntary movements. Lifestyle modifications play a vital role; regular physical activity enhances circulation, while stress-reduction techniques like yoga, meditation, and adequate sleep can help manage symptoms. In more severe cases, advanced interventions like deep brain stimulation (DBS) are available, which can significantly reduce involuntary movements in selected patients. Preventive strategies, such as routine monitoring of neurological status and patient education, are essential components of comprehensive care.
Safety considerations are paramount, especially for older adults who are more vulnerable to injuries resulting from involuntary movements. Creating a safe environment—removing tripping hazards, using supportive devices, and ensuring proper lighting—can help prevent falls and injuries. Engaging in ongoing research to better understand the pathophysiology of TD and improve treatment options remains important. Ultimately, multidisciplinary approaches involving neurologists, psychiatrists, physical therapists, and caregivers provide the best outcomes for managing tardive dyskinesia effectively.