Comprehensive Guide to Allergies and Asthma: Causes, Risks, and Effective Management Strategies
This comprehensive article explores how allergies can trigger asthma symptoms, highlighting causes, risk factors, and effective management methods. It emphasizes the importance of identifying triggers like pollen, pet dander, and dust, and offers practical tips such as environmental control and medical treatment options to help those affected control allergy-induced asthma. Understanding this connection can lead to better prevention strategies, reducing the frequency and severity of asthma attacks caused by allergies, improving quality of life for sufferers.

Understanding the Intersection of Allergies and Asthma
There is a common misconception that allergies and asthma are completely separate health conditions. However, in reality, allergies play a significant role in the development and exacerbation of asthma symptoms. Allergic reactions can often trigger asthma attacks, highlighting the close connection between these two respiratory issues. This article delves into the relationship between allergies and asthma, elaborates on the primary causes, discusses risk factors, and provides comprehensive strategies for managing allergy-induced asthma effectively.
If you or a loved one suffer from allergies, understanding how these sensitivities influence asthma can lead to better control and improved quality of life. Recognizing the common triggers like pet dander, pollen, and dust, as well as learning about preventive measures, can help reduce the frequency and severity of asthma attacks related to allergies.
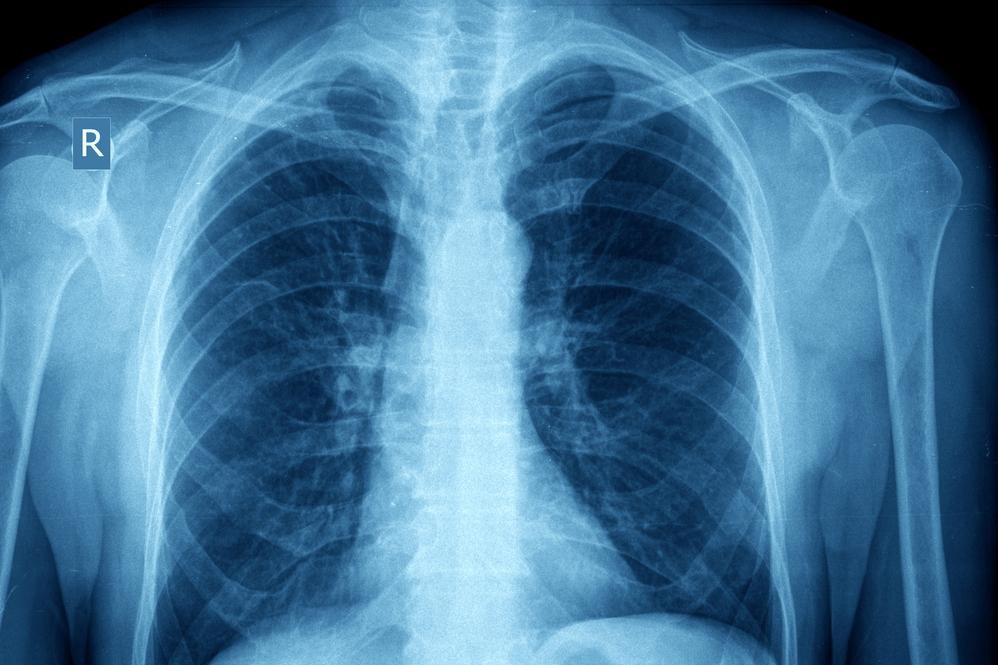
The pathway from allergies to asthma involves complex immune responses. When the immune system erroneously perceives harmless substances—such as pet hair, pollen, dust mites, or mold—as threats, it responds by releasing antibodies. This immune response leads to allergic inflammation in the respiratory tract. For individuals with asthma, this inflammation causes narrowing of the airways, resulting in symptoms such as wheezing, coughing, chest tightness, and difficulty breathing. This allergy-driven airway constriction is classified as allergy-induced or allergic asthma.
Research indicates that a substantial proportion of asthma cases are linked to allergic sensitivities. It is estimated that approximately 80% of asthma patients also experience pollen allergies, underlining the strong connection between seasonal allergies and asthma flare-ups. Moreover, a family history of respiratory allergies or asthma can significantly increase an individual’s susceptibility to developing these conditions. Besides allergens, other factors such as stress, sudden temperature changes, physical exertion, and existing chronic health issues may also act as triggers.
Understanding the causes and triggers of allergy-related asthma is essential for effective management. The key to control lies in minimizing exposure to known allergens and employing appropriate medical interventions. Over-the-counter antihistamines can help alleviate allergic symptoms, while wearing masks during high pollen seasons can reduce inhalation of airborne allergens. Monitoring local pollen counts and staying indoors during peak allergen times further decreases risk. Keeping your living environment clean by replacing air filters regularly, reducing mold growth, and vacuuming frequently can diminish indoor allergens significantly.
In addition, personalized treatment plans recommended by healthcare providers include options such as nasal sprays, antihistamines, inhalers, and immunotherapy, which can help desensitize the immune system to specific allergens. Regular medical checkups are crucial to evaluate the severity of reactions and adjust treatments accordingly. With a proactive approach, many individuals can manage their allergy-induced asthma effectively, leading to fewer attacks, less medication use, and better overall respiratory health.